Cell子刊:中科院上海药物研究所徐华强团队等揭示5-HT受体配体识别和G蛋白选择调控机制!
2022-08-18 转化医学网 转化医学网
揭示了A类GPCR选择性偶联G蛋白的分子机制,填补了5-HT家族受体结构分析的空白。
导读:最新研究揭示了A类GPCR选择性偶联G蛋白的分子机制,填补了5-HT家族受体结构分析的空白。
这些对血清素受体的系统研究极大地丰富了我们对血清素系统的结构和功能的理解。由于抑郁症,精神分裂症和偏头痛可能与血清素有关,因此这项研究也可能有助于治疗这些疾病。
2022年6月16日,来自中科院上海药物研究所的徐华强团队,联合浙江大学张岩教授团队以及丹麦哥本哈根大学David E. Gloriam教授团队等,在《Molecular Cell》发表了题为“GPCRs steer Gi and Gs selectivity via TM5-TM6 switches as revealed by structures of serotonin receptors”的最新的研究成果。这是研究人员首次报告5-HT(血清素)的结构,并系统性地揭示了小分子配体5-HT和5-CT识别5-羟色胺受体亚型的结构基础,并阐明了5-羟色胺受体选择性偶联Gs蛋白和Gi蛋白的分子机制。
https://www.sciencedirect.com/science/article/abs/pii
01血清素和血清素受体
血清素 (5-HT) 是人类中枢神经系统和周围神经系统中的主要神经递质之一.它有助于通过血清素受体(5-HTR)调节食欲,记忆,认知和情绪。血清素受体家族是G蛋白偶联受体(GPCR)超家族中最复杂的亚家族之一,包含12个亚型。不同的受体亚型在人体内起着不同的生理作用,并与不同种类的G蛋白偶联。其中,5-HT4, 5-HT6和 5-HT7受体主要与下游G偶联s蛋白质和 5-HT1和 5-HT5受体主要与下游G偶联我蛋白质。

02研究方法过程概要
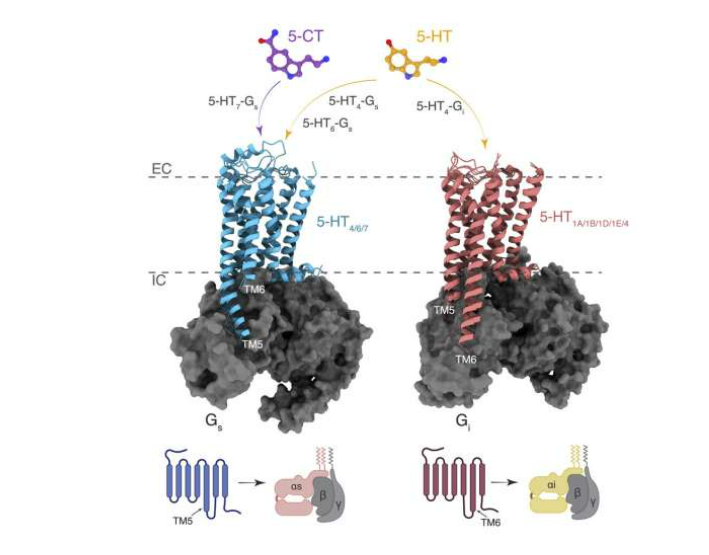
联合团队采用单颗粒冷冻电镜技术分别对5-HT激活5-HT4、5-HT6形成的Gs复合物、5-CT激活5-HT7形成的Gs复合物和5-HT激活5-HT4形成的Gi复合物进行了结构重塑,最终解析了4个在配体激活状态下与不同蛋白的复合物结构
该团队将所获的这三种Gs偶联的5-羟色胺受体与Gi偶联的5-羟色胺受体进行了结构比较,并进一步与另外已发表的19种Gs和Gi偶联的A类GPCRs结构进行比较。他们发现,跨膜螺旋TM5和TM6长度作为“macro-switch”来分别确定受体对Gs和Gi的选择性,且这种TM5-TM6 长度的“macro-switch”由A类GPCRs-G蛋白结构共享。此外,TM5和TM6中的特定残基充当“micro-switches”以与Gs或Gi形成特定的相互作用。

为探究G蛋白偏好5-羟色胺受体的假设,该团队进行了两组实验来检验TM5和TM6的长度是GPCR区分Gs和Gi蛋白的关键因素的假设。研究结果表明,嵌合受体5-HT1A (5-HT4_P5.50-P6.50)与野生型5-HT4具有相似的功能,即具有高组成型激活且几乎不受配体调节。同样,5-HT1A (5-HT7_P5.50-P6.50)显示出与野生型5-HT7相似的功能,在激动剂诱导下进行的cAMP 积累。如果将5-HT4和5-HT7的ICL3替换为5-HT1A,在激动剂诱导下进行的cAMP积累的能力几乎丧失,类似于野生型5-HT1A受体。综上所述,该团队以5-羟色胺家族受体为切入点揭示了A类GPCRs的Gs、Gi蛋白偶联选择性机制,并扩展了5-羟色胺受体的配体识别基础。
03研究成果及研究历程
徐华强团队长期致力于5-羟色胺家族受体的结构与功能研究,并取得了一系列系统性的重要成果。
2013年,在Science上首次报导了激动剂结合的5-HT1B受体的高分辨率晶体结构1。
2018年,在Cell Discovery发表了首个反向激动剂结合的5-HT1B受体的晶体结构2。
2021年3月,在Nature上首次报道了5-HT1A、5-HT1D、5-HT1E受体的结构,并揭示了磷脂PI4P(PtdIns4P)和胆固醇调节受体功能的机制和受体的本底激活机制3。
2021年7月,在Cell Research上首次报道了5-HT1F受体的结构,并揭示了偏头痛药物拉米替坦对该受体的选择性结合机制4。
2022年5月,在Cell Discovery上首次报道了5-HT5A受体的结构5。
这一最新成就不仅揭示了A类GPCR选择性偶联G蛋白的分子机制,而且还填补了5-HT家族受体结构分析的空白。这些对血清素受体的系统研究极大地丰富了我们对血清素系统的结构和功能的理解。由于抑郁症,精神分裂症和偏头痛可能与血清素有关,因此这项研究也可能有助于治疗这些疾病。
参考资料:
https://phys.org/news/2022-06-scientists-breakthrough-serotonin-receptors.html
http://www.simm.cas.cn/web/xwzx/kydt/202206/t20220617_6462601
注:本文旨在介绍医学研究进展,不能作为治疗方案参考。如需获得健康指导,请至正规医院就诊。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
76
#Cell#
77
#研究所#
48
#G蛋白#
34
#中科院#
37
#调控机制#
40