JAMA Surg:肿瘤破裂是影响局限性胃肠道间质瘤患者术后生存期的重要因素
2020-04-07 MedSci原创 MedSci原创
对于局限性胃肠道间质瘤患者,肿瘤破裂与否是影响患者总生存期的重要因素
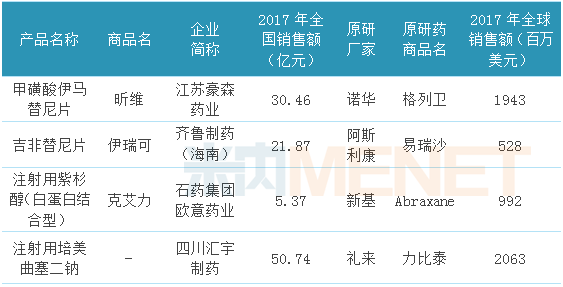
局限性胃肠道间质瘤(GIST)患者手术质量与整体生存率之间的关系尚不完全清楚。近日研究人员根据患者显微镜下边缘状态(R0/R1)评估术后接受伊马替尼与死亡风险的关系。
本次为III期临床研究的事后观察研究,中位随访9.1年,研究在12个国家的112家医院进行。原发性GIST,有中、高复发风险,手术后无疾病残留证据的成年患者参与,患者术后随机接受伊马替尼(400 mg/d)治疗2年或无辅助治疗。按中心、风险类别(高风险vs中等风险)、肿瘤部位(胃vs其他部位)、手术质量(R0 vs R1)分层。研究的主要终点为总生存率(OS)。
研究共纳入908例患者,其中男性465例,占51.4%,中位年龄59岁。162例(17.8%)接受R1切除术,162例(59.9%)中97例肿瘤破裂。对于接受R1 vs R0切除的患者,总体OS(危险比[HR]:2.05)和治疗后OS(伊马替尼组HR:2.65;无伊马替尼组HR: 1.86)有显著差异。排除肿瘤破裂后,R1和R0切除术的OS差异消失(HR:1.05)。
研究认为,对于局限性胃肠道间质瘤患者,肿瘤破裂与否是影响患者总生存期的重要因素。
原始出处:
Alessandro Gronchi et al. Quality of Surgery and Outcome in Localized Gastrointestinal Stromal Tumors Treated Within an International Intergroup Randomized Clinical Trial of Adjuvant Imatinib.JAMA Surg. April 1, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#局限性#
37
#胃肠道#
0
#生存期#
27
#间质瘤#
44
#肿瘤破裂#
33
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
61