JGH: 循环线粒体 DNA 水平升高可预测肝移植后患者的早期同种异体移植物功能障碍
2022-01-18 MedSci原创 MedSci原创
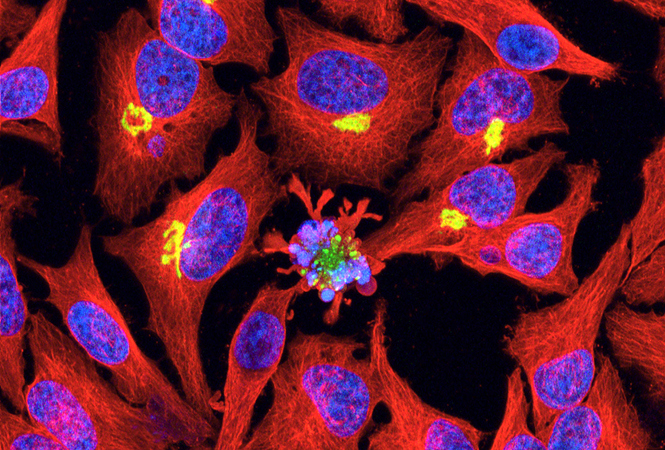
线粒体(mitochondrion)是一种存在于大多数细胞中的由两层膜包被的细胞器,是细胞中制造能量的结构,是细胞进行有氧呼吸的主要场所
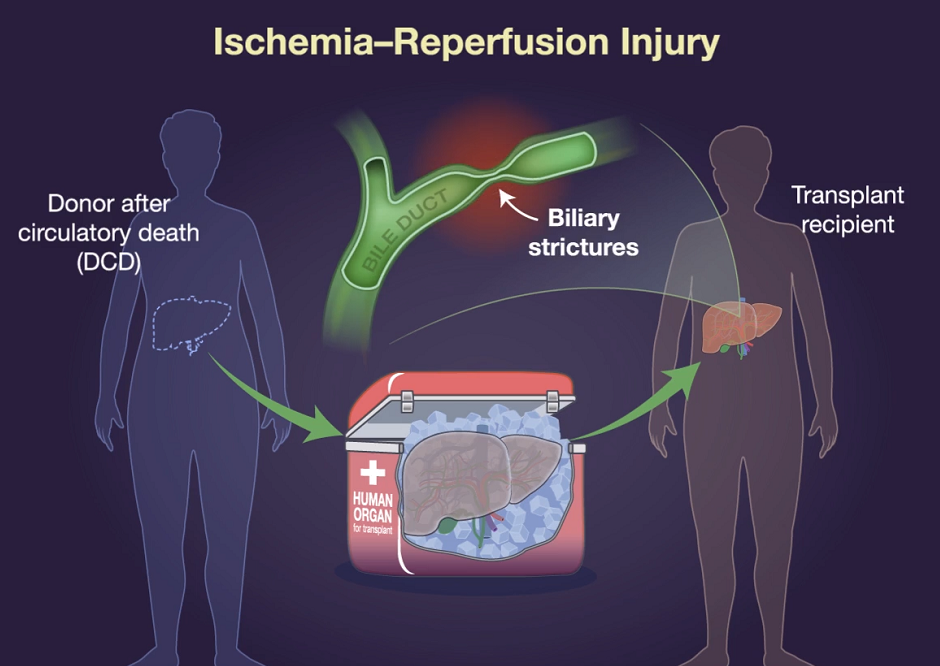
循环线粒体DNA(cmtDNA)的分析已受到关注,因为它有可能成为一些疾病中组织损伤和疾病负担的临床有用指标。 最近的工作表明,cmtDNA可以作为一种有效的与败血症、心肌缺血、慢性炎症性疾病有关的免疫调节剂。然而,它作为肝移植(LT)的生物标志物的作用和潜力仍有待阐明。早期异体移植功能障碍(EAD)是原发性移植功能障碍的一种较温和的形式,与术后并发症、较高的死亡率和移植物存活率下降有关。肝脏缺血和再灌注损伤被认为是导致EAD的肝细胞损伤的原因。移植后cmtDNA的作用和影响还不是很清楚。早期的研究发现,器官捐献者血样中cmtDNA水平的升高与移植后较高的并发症和死亡率有关。cmtDNA可能因肝损伤而释放到循环中;然而,最近的研究也表明cmtDNA是导致肝细胞损伤的原因。因此,研究人员假设升高的 cmtDNA 与肝移植 (LT) 后的不良事件有关,并进行了一项观察性队列研究。
研究人员收集了2019年9月至2020年2月期间在墨尔本的奥斯汀医院接受肝脏移植(LT)的21名患者。LT之后患者根据当地肝脏移植部门的指导方针进行生活管理,并进行至少6个月的随访。研究人员还招募了6名健康志愿者,以建立cmtDNA的对照组水平。血液样本被收集在含有EDTA的试管中,并在800g下离心10分钟然后再以3000g离心10分钟,以获得血浆部分。然后将血浆样品立即储存在-80°C进行cmtDNA分析。

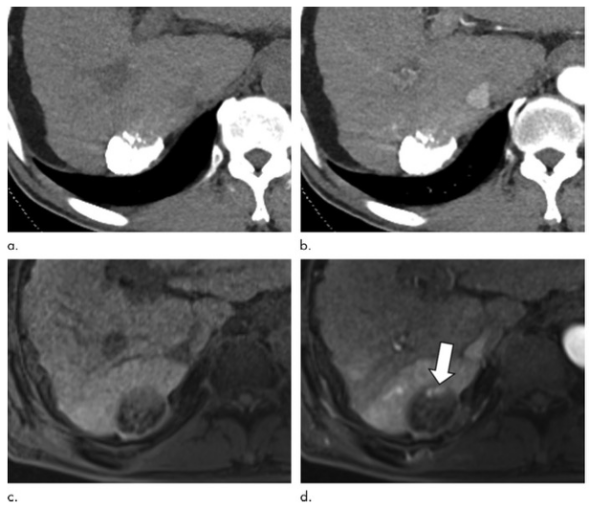
本项研究结果发现LT患者术后并发症发生率为 47.6%(n=10)。7 名患者 (33.3%) 有早期同种异体移植物功能障碍 (EAD),6 名患者 (28.5%) 在 LT 6 个月内出现急性细胞排斥反应。与健康对照和术前样本相比,LT 后所有受者的 cmtDNA 水平显着升高(1361937 拷贝/mL [IQR 586781–3 399687] VS 545 531拷贝/mL [IQR 238562–1 381015] ),并在移植后 5 天恢复到正常水平。术后早期出现EAD的患者cmtDNA水平尤其升高(P<0.001)。在所有患者中,最初 cmtDNA 与血浆肝细胞酶水平之间存在正相关性(P < 0.05)。然而,EAD 患者在术后第 7 天表现出 cmtDNA 的第二个峰值,但是这与肝功能无关。

图:循环线粒体 DNA水平与不同肝移植后患者中的差异
本项研究证实血浆cmtDNA的早期释放与肝细胞损伤密切相关;然而EAD患者中cmtDNA 的晚期激增似乎与肝细胞损伤无关。
原始出处:
Osamu Yoshino. Et al. Elevated levels of circulating mitochondrial DNA predict early allograft dysfunction in patients following liver transplantation. Journal of Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#同种异体#
47
#植物#
68
#功能障碍#
28
#异体移植#
31
#移植物#
39