房颤抗凝后为何还会发生中风?日本研究
2020-08-20 xujing 中国循环杂志
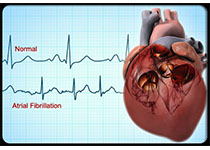
近日,Heart杂志发表的纳入11848例房颤患者的日本研究显示,房颤患者即使抗凝治疗有效,缺血性卒中和全身性栓塞的风险仍较高。
近日,Heart杂志发表的纳入11848例房颤患者的日本研究显示,房颤患者即使抗凝治疗有效,缺血性卒中和全身性栓塞的风险仍较高。
DOI:10.1136/heartjnl-2020-317299
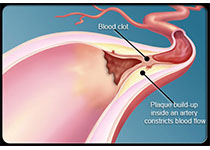
研究发现,高龄、高血压和血脂异常是房颤患者抗凝后发生缺血性卒中和全身性栓塞的危险因素。约三分之一的残余风险可归因于高血压、糖尿病和血脂异常。
该研究中,年龄<50岁者服用口服抗凝药的比例为39.1%,50~60岁为56.6%,60~65岁为61.0%,65~75岁为64.4%,抗凝药物的使用随着年龄的增长而增加。
平均随访3年,共发生200例缺血性卒中和全身性栓塞事件,发病率0.57%,仍然明显高于普通人群(0.1%-0.2%)。
在多变量分析中,≥65岁、高血压和血脂异常分别使缺血性卒中和全身性栓塞风险增加1倍、41%和46%。
研究发现,高血压、糖尿病和血脂异常,这三项可改变的危险因素导致的缺血性卒中和全身性栓塞风险占30%。
原始出处:Toshiki Maeda, Takumi Nishi, Shunsuke Funakoshi, et al. Residual risks of ischaemic stroke and systemic embolism among atrial fibrillation patients with anticoagulation: large-scale real-world data (F-CREATE project). Heart. online first, August 14, 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习
49
#房颤抗凝#
41
学习
80
学习了
98
学习
106
#日本#
0
房颤,临床上碰到很多哦
57
中风是俗称,应该称为缺血性卒中吧
40