iPSC疗法、新靶点、单细胞测序,帕金森病最新研究进展解读
2022-05-28 nagashi “生物世界”公众号
帕金森病的治疗和诊断一直是十分热门的研究领域,最近帕金森病领域有了一些新的突破。通过这篇文章,我们一起了解下帕金森病领域的一些新发现、新进展。
帕金森病(Parkinson's Disease,PD),是世界上第二常见的神经退行性疾病,仅次于阿尔茨海默病,在全世界影响着超过1000万人的生活,每年大约有60000名新患者确诊。虽然基于多巴胺的标准治疗可以在一定程度上缓解症状,但患者仍然会由于大脑黑质中多巴胺神经元的不断丢失,最终出现失能性运动障碍。
帕金森病的治疗和诊断一直是十分热门的研究领域,最近帕金森病领域有了一些新的突破。通过这篇文章,我们一起了解下帕金森病领域的一些新发现、新进展。
基于iPSC的帕金森疗法即将进入临床
2022年5月9日,美国生物技术公司 Aspen Neuroscience 宣布完成1.475亿美元的B轮融资,加速推进帕金森病的临床研究,这也将基于 iPSC 的帕金森病疗法再次带入公众视野。

自2018年成立以来,Aspen 公司已完成超过2.2亿美元融资。此次新一轮融资将重点推进其名为ANPD001的研究管线,这是一款基于诱导多能干细胞(iPSC)衍生自体神经元替代疗法,目前正在向 FDA 提交1/2a期临床试验申请。另一条研究管线则是针对遗传性帕金森病,目前处于早期研发阶段。

为什么帕金森病的iPSC疗法能引起如此高度的重视呢?
归根结底是因为传统的多巴胺疗法只能在一定程度上缓解症状,并不能从根本上解决问题,甚至对部分特殊帕金森患者完全无效。因此,这也促使医药界开发新的替代疗法。
有研究表明,在帕金森病诊断之前,黑质中就已经丢失了大约50%的多巴胺能神经元。基于多巴胺能神经元的细胞替代疗法具有释放多巴胺,重建神经网络的潜力。这种个性化的前沿疗法,可以从源头上直接修复多巴胺能神经元受损的大脑黑质,缓解甚至逆转帕金森症状,使帕金森患者重获新生。
预防帕金森病的神经退行性变
2022年5与10日,美国约翰斯·霍普金斯大学医学院的研究人员在 Cell 上发表题为:PAAN/MIF nuclease inhibition prevents neurodegeneration in Parkinson’s disease 的研究论文。
这项研究表明,病理性α-突触核蛋白(α-syn)诱导的神经退行性病变是通过 PAAN/MIF 核酸酶活性发生的。研究团队通过化合物筛选发现了一种可穿过血脑屏障的 PAAN/MIF 核酸酶抑制剂——PAANIB-1,它可以有效预防帕金森病的神经退行性变。

2007年,约翰霍普金斯大学医学院 Ted Dawson 与 Valina Dawson 夫妇发现了程序性脑细胞死亡的一种新形式,并将其命名为 Parthanatos,又称 PARP-1 依赖的细胞死亡。Parthanatos 死亡途径是基于 DNA 损伤和 PARP-1 激活的一种全新形式的程序性细胞坏死。
简单来说,在病理状态下,细胞中大量的 DNA 损伤导致 DNA 修复酶 PARP-1 被大量激活,PARP-1 会通过代谢通路抑制有氧呼吸过程,从而促使调亡诱导因子(AIF)释放并携带巨噬细胞迁移抑制因子(PAAN/MIF)入核,使染色质凝集和 DNA 大片段化,最终导致 Parthanatos 死亡。
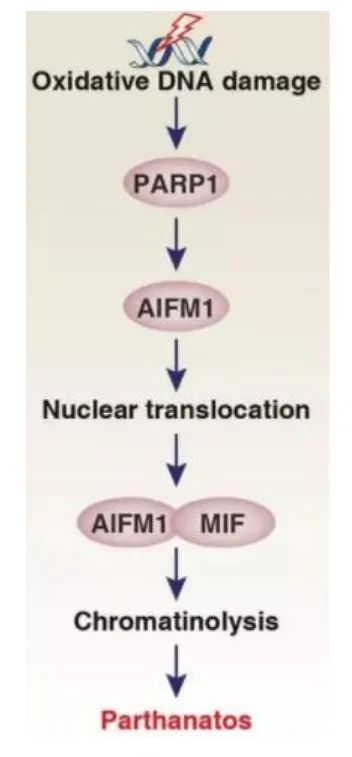
Parthanatos死亡途径
在另一方面,早在1912年,德国神经病学家 Frederic Lewy 在帕金森患者的脑组织中发现了一些异常的蛋白聚集,它们被命名为路易体(Lewy body)。1997年,英国剑桥大学神经生物学家 Michael Goedert 等发现了路易体的主要成分就是α-突触核蛋白。自此,科学家们开始将α-突触核蛋白与帕金森病联系在一起。
在这篇 Cell 论文中,研究团队首先证明了 Parthanatos 死亡途径中的 PAAN/MIF 核酸酶可以促使病理性α-突触核蛋白的形成。当研究人员将 PAAN/MIF 基因缺失或构建其缺乏核酸酶活性的突变体时,可以帕金森病小鼠模型的多巴胺能神经元的缺失和行为缺陷。
更重要的是,研究团队通过化合物筛选发现了 PAANIB-1,一种可穿越血脑屏障的 PAAN/MIF 核酸酶抑制剂,可预防 α-syn 预制纤维(α-Syn PFF)、AAV-α-syn 过表达或 MPTP 中毒等机制诱导的帕金森病小鼠模型中的神经退行性变。

研究模式图
这些发现表明 Parthanatos 死亡途径相关的 PAAN/MIF 核酸酶抑制剂可能是治疗帕金森病的潜在药物,为新的帕金森治疗方案的出现奠定基础。
单细胞测序时代的帕金森病
大脑黑质的多巴胺能神经元病变是帕金森病的病理标志,然而,科学家们也观察到黑质致密部(SNpc)的一些神经元甚至可以存活到帕金森病的晚期阶段,这表明不同的黑质神经元对帕金森病导致的神经退化具有差异性。
对此,更清楚地了解脆弱神经元的特定分子特征,以及导致其死亡的相关分子级联事件,可以为完善帕金森病的实验室模型提供机会,并有助于改善帕金森病的预后或发展细胞类型特异性治疗。
2022年5月5日,Broad 研究所的研究人员在 Nature Neuroscience 期刊上发表题为:Single-cell genomic profiling of human dopamine neurons identifies a population that selectively degenerates in Parkinson's disease的研究论文。

该研究开发了一种选择性富集死亡帕金森患者黑质致密部的多巴胺能神经元的方法,并在富集后通过单细胞核RNA测序(snRNA-seq)对这些来自帕金森病患者的多巴胺能神经元进行转录谱分析,以此确定了10个不同的多巴胺能神经元亚群。
研究团队还通过一种高分辨率空间转录组学技术——Slide-seq,沿着黑质致密部的背侧-腹侧轴对这些细胞亚群进行了空间定位。他们发现,一个以 AGTR1 基因表达为标志的多巴胺能神经元亚群在帕金森病中高度易损,它们在空间上位于黑质致密部的腹侧层,并表现出最强的 TP53 和 NR2F2 上调。

snRNA-seq确定10个多巴胺能神经元亚群
更关键的是,这类帕金森病易损细胞的转录特征与之前的全基因组关联分析(GWAS)帕金森病高表达基因高度重合。这表明,细胞内的一些分子机制可能在某些多巴胺能神经元亚群对帕金森病的选择脆弱性中起着重要作用。
这项基于单细胞转录组测序的发现,有助于人们更好地理解帕金森病的病因,找到在帕金森病中易损的多巴胺能神经元,这对于测试帕金森病新药或疗法的效果有着积极的意义。
总而言之,帕金森病仍有许多谜题等着我们去解答,无论是 iPSC 衍生的帕金森病自体神经元替代疗法的临床推进,还是 Parthanatos 死亡途径、α-突触核蛋白和帕金森病的联系。这些最新进展都提醒我们,仍需要加快脚步,继续探索未知的领域,人类才能彻底攻克帕金森病乃至其他的神经退行性疾病。
参考文献:
1.https://doi.org/10.1016/j.cell.2022.04.020
2.https://doi.org/10.1038/s41593-022-01061-1
3.https://www.nature.com/articles/s41593-022-01069-7
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#最新#
47
#单细胞测序#,#帕金森病#
114
#新靶点#
33
#iPS#
39
#研究进展#
38
#PSC#
35
#iPSC#
43