SCI REP:多次新鲜粪便微生物移植诱导并维持Crohn病并发炎症性肿块的临床缓解!
2017-07-07 xing.T MedSci原创
这种务实的研究表明序贯新鲜的FMTs可能是一种有效、安全的治疗方法来诱导和维持有腹腔内炎性包块的CD患者的临床缓解。
中国古代医学文献以及我国现有的临床经验表明,粪便菌群移植(FMT)可以治疗炎性肿块。近日,Scientific reports 杂志上发表了一篇研究文章,研究人员的目的是评估多次新鲜FMTs来治疗克罗恩病(CD)并发腹腔炎性肿块。
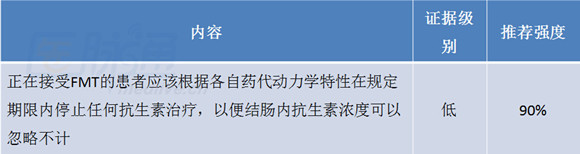
该研究的所有患者遵守“一小时的FMT协议”。二十五例患者经CT或MRI被诊断为CD及相关炎性肿块。所有患者均接受最初的FMT后每3个月重复一次FMT。该研究的主要终点是临床反应(改善和缓解),并在12个月内持续临床缓解。该研究的次要终点是基于横断面成像和FMT的安全性的脓肿大小的改善。
研究人员发现在接受最初的FMT后3个月分别有68%(17/25)和52%(13/25)的患者达到了临床反应和临床缓解。序列FMTs在6个月、12个月和18个月达到持续临床缓解的患者比例分别为48%(12/25)、32%(8/25)和22.7%(5/22)。9.5%(2/21)的患者达到放射治愈,71.4%(15/21)的患者达到放射学改善。没有观察到FMT相关的严重不良事件。
这种务实的研究表明序贯新鲜的FMTs可能是一种有效、安全的治疗方法来诱导和维持有腹腔内炎性包块的CD患者的临床缓解。
原始出处:
Zhi He, Pan Li,et al. Multiple fresh fecal microbiota transplants induces and maintains clinical remission in Crohn’s disease complicated with inflammatory mass.Scientific reports. 2017. https://www.nature.com/articles/s41598-017-04984-z
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Crohn病#
20
#粪便微生物#
26
#微生物#
31
#CRO#
31
#Crohn#
23
#临床缓解#
37
#并发#
18
很好,不错,以后会多学习
62
粪便微生物移植。
53
很好,不错,以后会多学习
48