Cancers:新生儿筛查TP53 R337H变异检测和监测儿童肾上腺皮质肿瘤的早期诊断
2022-01-14 从医路漫漫 MedSci原创
巴西南部儿童肾上腺皮质肿瘤(ACT)的发病率约为世界其他地区的20倍。人群中TP53 R337H变异的存在导致了ACT和其他儿童肿瘤病例数量的增加。
背景:巴西南部儿童肾上腺皮质肿瘤(ACT)的发病率约为世界其他地区的20倍。人群中TP53 R337H变异的存在导致了ACT和其他儿童肿瘤病例数量的增加。在儿童ACT中,生殖系TP53和β-catenin (CTNNB1)激活突变的同时发生是罕见的。在一项使用两种不同队列和方法(71例ACT儿童病例)的研究中,激活β-catenin突变(n = 13)仅在野生型TP53个体(n = 35)中检测到,而在生殖系TP53突变个体(n = 36)中均未检测到。一种可靠且廉价的检测血液中TP53 R337H杂合子的基因检测方法的存在,使得筛查新生儿成为识别R337H携带者的合理方法。新生儿R337H携带者筛查/监测(NSS)包括密切的临床观察、肾上腺皮质激素血药浓度监测和影像学研究,效果良好,显示了监测对早期诊断和干预的有效性。在发病的前10年,ACT的累积风险约为4%,并逐渐下降。在一般人群中,这一年龄组的累积发病率比患有任何类型癌症的儿童高25倍。携带R337H变异的儿童患其他癌症的风险,特别是神经母细胞瘤和骨肉瘤的风险略高于普通人群。在携带R337h的家族中,晚发型(成人)肿瘤比儿童肿瘤更常见。ACT的监测是否有助于该年龄组其他儿童肿瘤的早期诊断仍不清楚。此外,监测工作复杂而昂贵,需要经常到医院就诊并抽血进行激素检测和影像学研究。Li-Fraumeni综合征的监测检测结果可能存在假阳性或假阴性,尽管这种情况很少见。然而,在大型纵向研究中考虑这种可能性是很重要的。密集监测对携带者状况的间接影响包括参与者因频繁抽血、影像学研究、就诊旅行、缺课、日常活动中断和心理伤害而造成疼痛和不适。
方法:本研究对未参加新生儿筛查(非NSS)的ACT患儿的医疗记录进行了回顾(2012-2018)。我们比较了新生儿筛检/监测(NSS)和非NSS队列之间的已知预后因素以及估计的监测和治疗费用。
结果:在16名携带R337H变异的非NSS儿童中,分别有5名、5名、1名和5名儿童观察到肿瘤分期为I、II、III和IV期。肿瘤重量22~608g,11例ACT患儿均为I期,均存活。NSS组的中位肿瘤重量、诊断年龄和症状与诊断的间隔时间分别为21g、1.9年和2周,而非NSS组的中位肿瘤重量、诊断年龄和症状与诊断的间隔时间分别为210g、5.2岁和15周。每名患者每年挽救生命的监测/筛查成本估计为623美元。
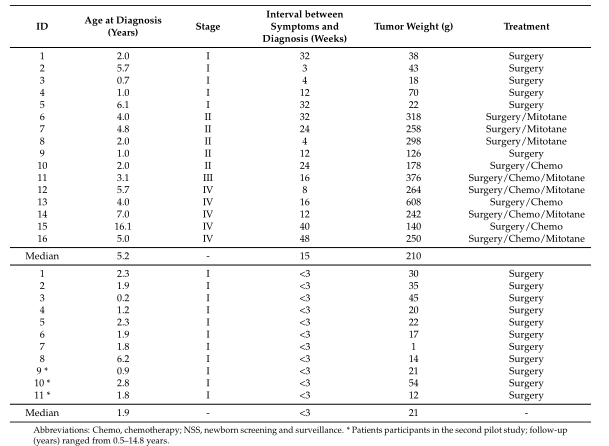
表1 2011年至2019年在一家医院住院的病例特征(非nss);较低:新生儿筛查和监测(NSS)发现肿瘤参与者的特征。
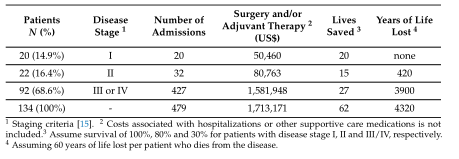
表2 2006年至2019年在公立医院诊断ACT的儿童DATASUS注册数据。
结论:在2006年至2019年期间登记的134例儿童ACT病例的分析的证实,该数据库包括来自农村和城市地区的病例,表明只有15%的病例处于第一阶段ACT。诊断时的疾病程度是与ACT术后预后相关的最重要的单一变量。I期ACT患者(完全切除肿瘤,重量< 100 g)无病生存的概率较高,肿瘤< 50 g的无病生存概率接近100%。相反,转移性(IV期)或术后残留病变(III期)患者疾病进展率高,预后差。最后,II期患者复发率较高,但仍可通过额外手术和强化化疗治愈。延误诊断与更高比例的II, III和IV阶段有关,由于这些孩子的躯体增长,可能与性早熟混淆。当注意到与雄激素(男性化)或皮质醇(库欣综合征)生产过剩相关的明显体征和症状时,肿瘤已经进展到I期以上。几乎所有重量< 50克的ACT分泌激素都会产生引起临床表现,这很容易引起重视,,这些肿瘤通常被完全切除和根除。因此NSS对改善该地区儿童ACT的预后至关重要。因此,我们强烈主张将R337H纳入国家规定的全民筛查和监测。
原文出处:Tosin KCF, Legal EF, Pianovski MAD,et al.TP53Newborn Screening for the Detection of the R337H Variant and Surveillance for Early Diagnosis of Pediatric Adrenocortical Tumors: Lessons Learned and Way Forward.Cancers (Basel) 2021 Dec 03;13(23)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#新生儿筛查#
36
#ERS#
19
#肾上腺#
24
#变异#
20
#p53#
41
#早期诊断#
39
#TP53#
52