拜耳的Nubeqa获得NICE支持,用于治疗前列腺癌
2020-10-27 Allan MedSci原创
Nubeqa(darolutamide)已被授权与雄激素剥夺疗法(ADT)一起使用。根据拜耳的说法,这是NICE在这种适应症中推荐的第一种治疗方法。
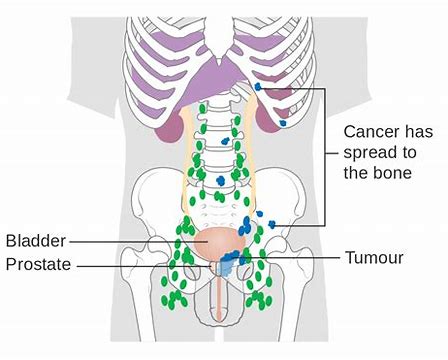
前列腺癌是英国男性中最常见的癌症,平均每年有48,000多例新病例。在患有非转移性去势抵抗性前列腺癌(nmCRPC)的男性中,约有三分之一在两年内发生转移,这凸显了这类患者的医疗需求。
拜耳的Nubeqa在治疗非转移性去势抵抗性前列腺癌(nmCRPC)方面获得了英国国家健康与护理卓越研究所(NICE)的支持。Nubeqa(darolutamide)已被授权与雄激素剥夺疗法(ADT)一起使用。根据拜耳的说法,这是NICE在这种适应症中推荐的第一种治疗方法。
NICE的推荐是基于ARAMIS III期试验的结果,该试验评估了Nubeqa联合ADT治疗nmCRPC患者的疗效和安全性。在该试验中,Nubeqa联合ADT在无转移生存(MFS)的主要疗效终点方面显示出统计学上的显著改善,中位值为40.4个月,而安慰剂联合ADT仅为18.4个月。总体生存(OS)数据(表明,与安慰剂联合ADT相比,Nubeqa联合ADT组患者的OS得到显著改善,死亡风险降低了31%。
原始出处:
http://www.pharmatimes.com/news/bayers_nubeqa_wins_nice_prostate_cancer_backing_1354813
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#NICE#
35
#拜耳#
33
很不错
97
前列腺癌相关研究,学习了,谢谢梅斯
46
学习了,谢谢分享
103
继续学习了
88
学习了
107