J Clin Oncol:利妥昔单抗联合来那度胺或化疗治疗滤泡性淋巴瘤的长期预后
2022-08-12 MedSci原创 MedSci原创
在既往未治疗过的晚期滤泡性淋巴瘤患者中,R2方案显示出了与R-化疗方案相当的、持久的疗效和安全性,可成为无化疗的替代方案
免疫化学疗法仍然是需要全身治疗的滤泡性淋巴瘤 (FL) 患者的一线金标准;但是,目前已证明 FL 对非化疗方案有免疫反应。来那度胺是一种具有多种特性的免疫调节剂,包括改变细胞因子的产生,增加 T 细胞共刺激和自然杀伤细胞的细胞毒性。已有临床试验证明,来那度胺和利妥昔单抗(即 R2)联合使用在既往未治疗的 FL 患者中显示出有希望的活性和高反应率。
RELEVANCE 试验是一项3期的临床试验,旨在比较来那度胺+利妥昔单抗(R2) vs 利妥昔单抗+化疗(R-化疗)在既往未治疗过的晚期 FL 患者中的疗效和安全性。本文报告了该试验随访6年后的二次分析结果。
在该试验中,1-3a 期 FL 患者被随机(1:1)分至 R2 组或 R-化疗组,继以利妥昔单抗维持。主要终点是120周时的完全缓解率和无进展生存率(PFS)。
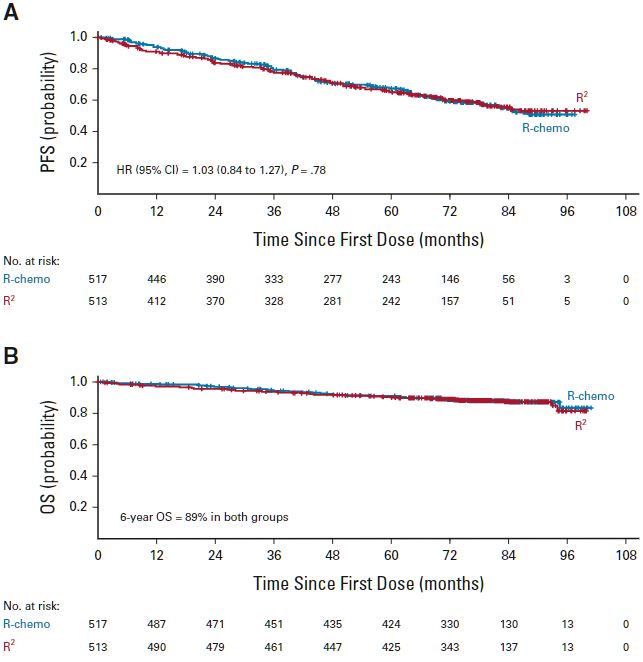
两组的PFS和OS
中位随访了72个月后,R2 组和 R-化疗组的6年 PFS 分别是60%和59%(风险比[HR] 1.03)。两组的6年总生存率均估算为89%。两组的中位无进展生存期和总生存期均尚未达到。
R2 组和 R-化疗组进展后的总缓解率分别是61%和59%,进展后的5年估算生存率分别是69%和74%。R2 和 R-化疗组每年的转化率分别为 0.68% 和 0.45%,继发原发性恶性肿瘤的发生率分别是11%和13%(p=0.34)。未观察到新的安全信号。
综上,在既往未治疗过的晚期滤泡性淋巴瘤患者中,R2方案显示出了与R-化疗方案相当的、持久的疗效和安全性,可成为无化疗的替代方案。
原始出处:
Franck Morschhauser, et al. Six-Year Results From RELEVANCE: Lenalidomide Plus Rituximab (R2) Versus Rituximab-Chemotherapy Followed by Rituximab Maintenance in Untreated Advanced Follicular Lymphoma. Journal of Clinical Oncology. August 10, 2022. https://ascopubs.org/doi/full/10.1200/JCO.22.00843.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#长期预后#
38
#Oncol#
40
#利妥昔#
46
#滤泡性淋巴瘤#
53
非常好的文章
44