JCO:男性甲状腺乳头状癌预后是否更差?BRAF V600E突变说了算
2018-08-12 国际循环编辑部 国际循环
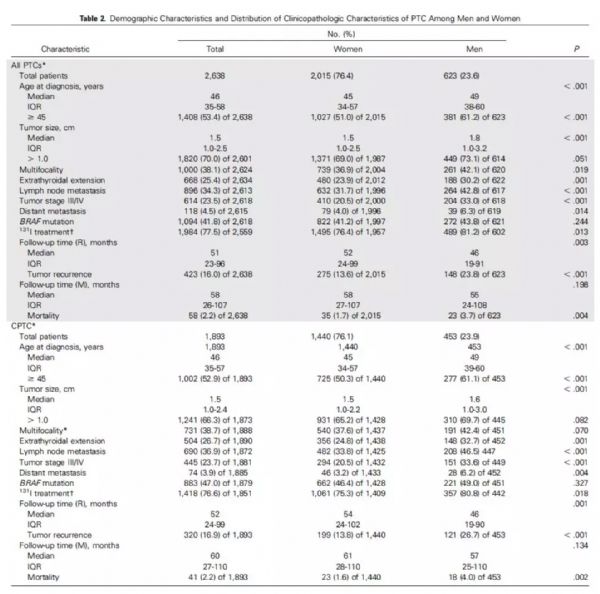
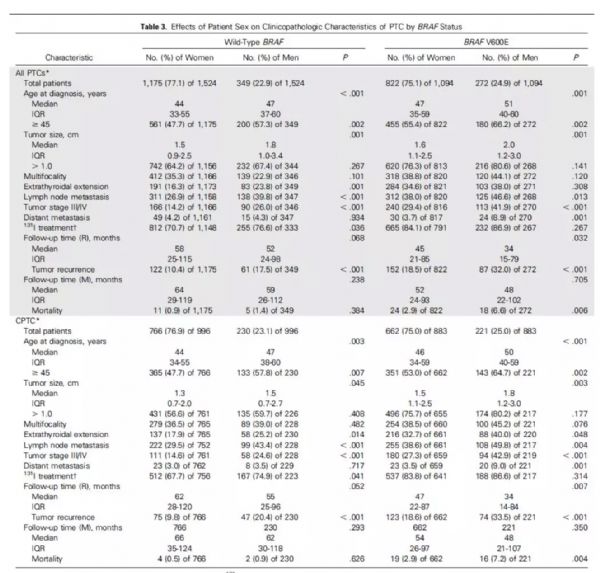
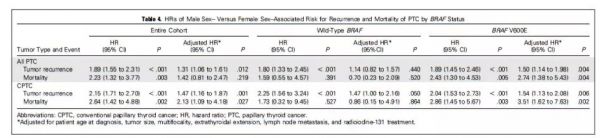
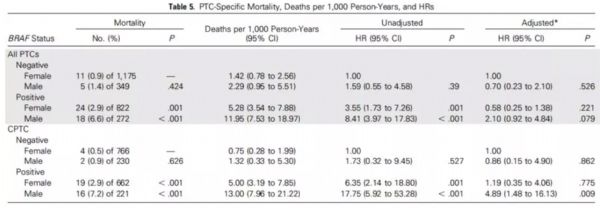
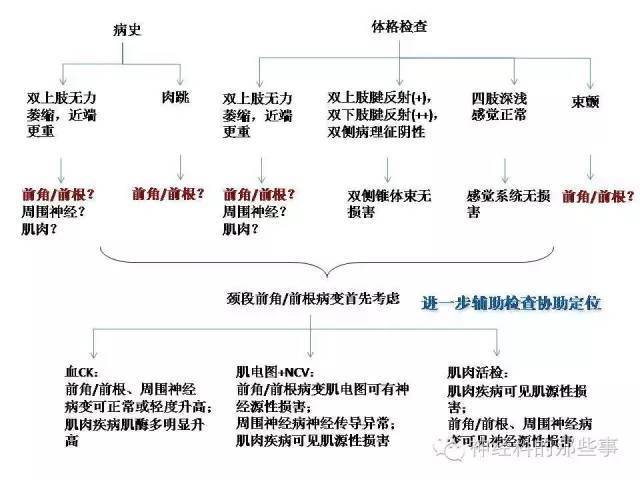
大多数甲状腺乳头状癌患者表现为惰性生长,但也有部分患者表现为侵袭性疾病,如何个体化的管理甲状腺乳头状癌患者是临床的热点,这就有赖于合适的风险分层,尤其是对患者死亡风险的分层。既往的研究发现男性可能是甲状腺乳头状癌预后的独立危险因素,但各个研究结果报道不一,尚无定论。近日发表在JCO杂志的一项研究,根据患者的BRAF V600E突变状态进一步分子,评估男性是否为甲状腺乳头状癌的独立预后因素。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










谢谢分享!很有用
68
#V600E突变#
0
#乳头状#
29
#JCO#
32
#BRAF#
36
#甲状腺乳头状癌#
41
学习了谢谢
73
学习了,谢谢分享。
91
学习了,谢谢分享
58