JCEM:白细胞端粒长度与甲状腺乳头状癌风险
2019-03-01 xing.T 网络
由此可见,该研究结果表明RTL与PTC的易感性显著相关。端粒长度和PTC风险之间存在明显的反向U形关联。端粒长度可能是一种潜在的、有价值的生物标志物,用于识别具有PTC高风险的个体。
端粒长度可能导致乳头状甲状腺癌(PTC)易感性。近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,该研究旨在验证一个假设,即白细胞端粒长度与PTC风险之间的关系。
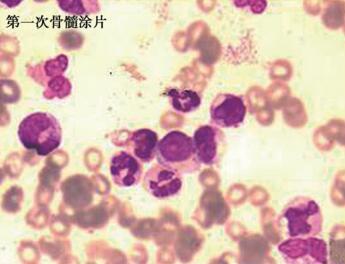
该研究为中国汉族人群病例对照研究,共纳入了1200名PTC患者和1201名年龄和性别匹配的健康对照者。研究人员通过Logistic回归计算了比值比(OR)和95%置信区间(CI)。
较短的相对端粒长度(RTL)与PTC风险升高显著相关(OR=1.61,95%CI为1.35-1.92,P=1.30×10-7)。有趣的是,当根据对照者RTL四分位数分布将个体分为四组时,研究人员观察到端粒长度与PTC风险之间存在反向U形关联。与作为参考组的第一个四分位数(最长的)相比,第二、第三和第四(最短)四分位数的个体ORs(95%CI)分别为5.61(4.04-7.78)(P=6.10×10-25)、9.33(6.78-12.83)(P=6.99×10-43)和1.23(0.83-1.81)(P=0.300)。这种反向U形关联在年轻人中更为明显。
由此可见,该研究结果表明RTL与PTC的易感性显著相关。端粒长度和PTC风险之间存在明显的反向U形关联。端粒长度可能是一种潜在的、有价值的生物标志物,用于识别具有PTC高风险的个体。
原始出处:
Ji Li.et al.Leukocyte telomere length and risk of papillary thyroid carcinoma.J Clin Endocrinol Metab. 2019.https://doi.org/10.1210/jc.2018-02471
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JCE#
30
#JCEM#
39
#癌风险#
35
#乳头状#
27
#端粒长度#
38
#甲状腺乳头状癌#
34
为作品点赞!认真学习了,把经验应用于实践,为患者解除病痛。
71