J Urol:男性癌症患者的射精障碍:患病率的系统回顾和元分析
2021-08-09 AlexYang MedSci原创
癌症是全球第二大死因。2018年估计有960万人因癌死亡,占死亡人数的六分之一。癌症负担在全球范围内持续增长。
癌症是全球第二大死因。2018年估计有960万人因癌死亡,占死亡人数的六分之一。癌症负担在全球范围内持续增长。早期检测、高质量的治疗和幸存者护理使得许多类型癌症的存活率正在提高。肺癌、前列腺癌、结肠直肠癌、胃癌和肝癌是男性最常见的癌症类型,对身体和心理都有广泛的不利影响,包括与疾病以及治疗引起的性功能有关的影响。反过来说,性功能的恶化与焦虑、情绪低落以及个人和夫妻生活质量的下降有关。

癌症治疗后的射精功能障碍(EjD)和勃起功能障碍是临床上重要的并发症,但它们在各种癌症部位和治疗类型中的确切发病率尚不清楚。近期,有研究人员进行了系统回顾和元分析,对现有的证据进行了调查,提供与所有癌症部位有关的射精障碍和勃起功能障碍的流行率的汇总估计,并确定与癌症患者射精障碍相关的特征。
研究人员搜索了四个电子数据库(Medline、CINAHL、PsychInfo和Embase),截至日期为2020年7月22日。所有报告男性癌症患者中EjD患病率的回顾性或前瞻性研究均纳入该综述中。他们还进行了随机效应元分析,计算患病率和95%置信区间(CIs)。根据癌症部位和治疗类型,计算了EjD的发病率比例。
共有64项研究(共10,057名参与者)纳入分析。最常见的癌症部位是膀胱、结肠、睾丸和直肠。手术干预后EjD的流行率从结肠癌的14.5%(95% CI 2.2-56.3%)到膀胱癌的53.0%(23.3-80.7%)。勃起功能障碍的患病率从膀胱癌的6.8%(95% CI 0.8-39.1%)到直肠癌的68.7%(95% CI 55.2-79.6%)。
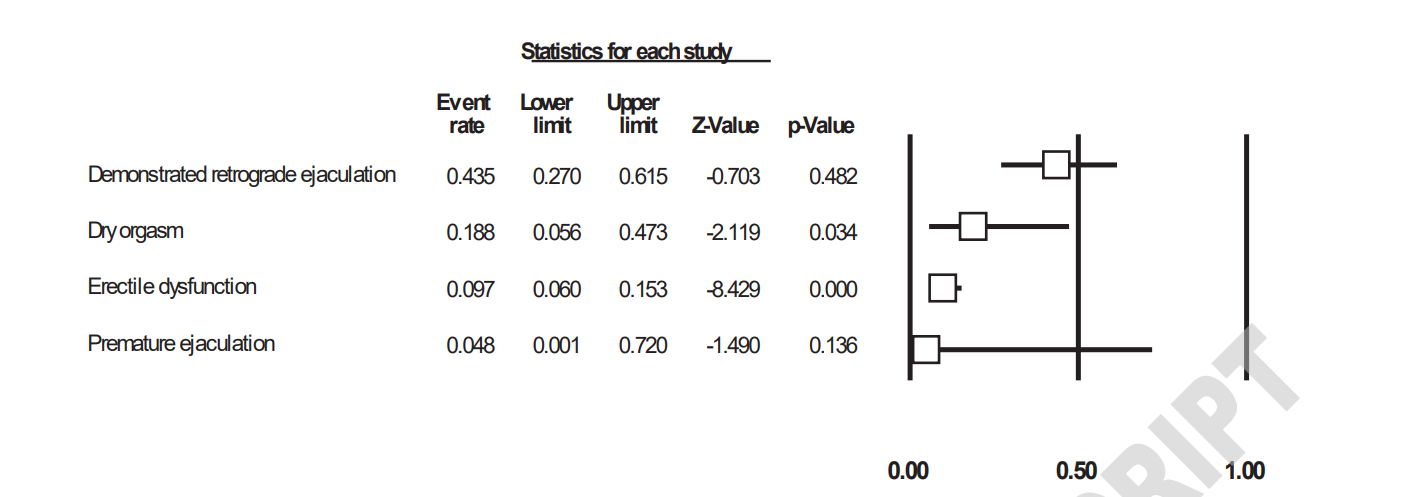
睾丸癌术后治疗的各种射精障碍的汇集发病率
综上所述,在该大型研究层面的元分析中,他们观察到了不同癌症部位和不同治疗类型的射精障碍和勃起功能障碍患病率高。因此,有必要对各种癌症治疗后的射精障碍和勃起功能障碍进行前瞻性研究。
原始出处:
Damiano Pizzol, Mike Trott , Igor Grabovac et al. Ejaculation Disorders in Male Patients With Cancer: A Systematic Review and Meta-Analysis of Prevalence. J Urol. Jul 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#射精障碍#
54
#元分析#
37
#患病率#
47
#癌症患者#
50
#射精#
42
#系统回顾#
37