罗氏CD20利妥昔单抗治疗寻常型天疱疮的III试验成功
2019-10-18 MedSci MedSci原创
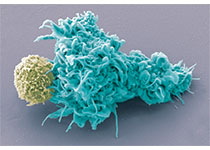
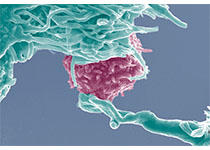
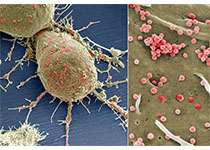
罗氏(Roche)发布III期研究PEMPHIX的数据,该研究评估了在中度至重度寻常型天疱疮的成年患者中,美罗华(利妥昔单抗)与霉酚酸酯(MMF)相比的药效和安全性。该研究在第52周达到了其主要终点,并证明Rituxan优于MMF,接受利妥昔单抗治疗的患者中40.3%无需使用类固醇即可达到持续完全缓解(CR)16周或更长时间。 利妥昔单抗在所有次要终点的统计学上也都有利,例如较低的口服糖
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#III#
35
#寻常型天疱疮#
45
#寻常型#
31
#III试验#
28
#CD20#
40
#利妥昔#
24
学习了谢谢分享
111