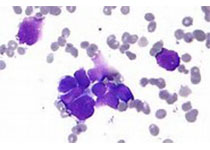
PNAS:破解PD-1抗体促进癌症超进展之谜!日本科学家发现PD-1抗体可激活调节T细胞,导致癌症超进展
2019-05-12 奇点糕 奇点网
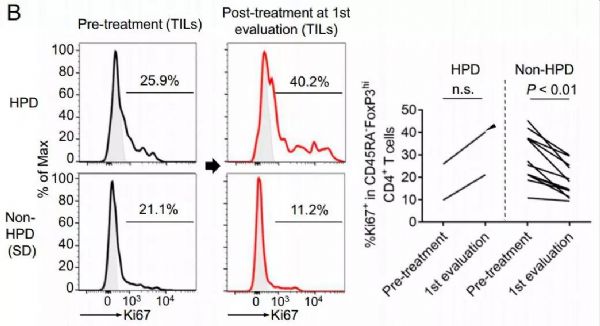
之前的一项研究数据显示,多癌种的晚期患者中,9%(12/131)在PD-1单抗治疗期间死于HPD。此前我们报道的韩国研究则显示,晚期非小细胞肺癌患者中HPD发生的比例为18.9%。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#科学家发现#
39
#超进展#
44
#本科#
32
#调节T细胞#
31
一定是PD_1表达高的对于免疫治疗才有效果?
72
#PNAS#
28
#日本#
22
#致癌#
24
#PD-1抗体#
25
好好好真的好
70