Eur Heart J:乳腺癌患者房颤的发生率、危险因素和死亡情况
2021-11-15 MedSci原创 MedSci原创
女性确诊乳腺癌后AF发生率明显更高。诊断时较高的乳腺癌分期与较高的AF风险显著相关。在新的乳腺癌诊断中,新发AF会增加1年心血管死亡率,但不会增加与乳腺癌相关的死亡率。
在多民族代表性的美国乳腺癌患者队列中,房颤(AF)的发病率、患病率、危险因素和死亡结局尚未明确。近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究的目的是评估乳腺癌患者AF的全国发病率、危险因素和相关死亡率。

研究人员使用监测、流行病学和最终结果与医疗保险相关的数据库,确定了2007年至2014年期间66岁以上新的主要诊断为乳腺癌的女性。这些患者分别与没有癌症的医疗保险参保人1:1匹配,每对随访1年以确定AF的主要结局。

研究人员使用竞争风险生存统计计算了累计发生率。在此之后,研究人员使用调整后的Cox比例风险模型确定乳腺癌患者AF的危险因素。最后,研究人员使用Kaplan-Meier方法和调整后的Cox比例风险模型估计新发和患有AF的乳腺癌患者的死亡率。
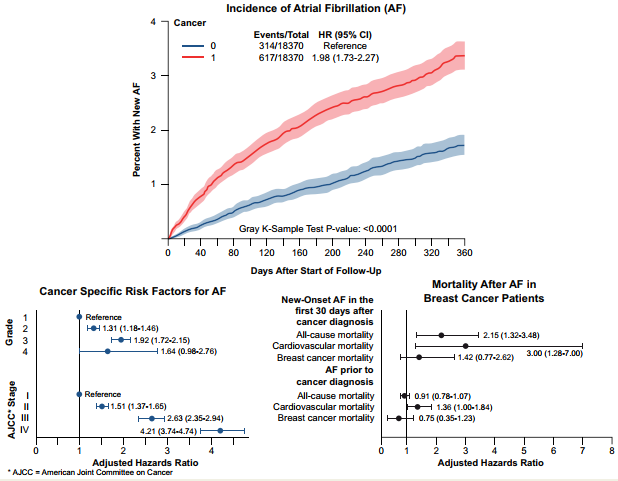
该研究纳入了85423名乳腺癌患者,其中9425名(11.0%)患者在乳腺癌诊断前就已诊断为AF。在乳腺癌诊断后的1年内,2993名(3.9%)患者被诊断出新发AF[发生率为3.3%,95%置信区间(CI)为3.0-3.5%;前60天(0.6%/月)的比值比更高]。相比之下,在匹配的非癌症对照者中新发AF的发生率为1.8%(95%CI为1.6-2.0%)。除了传统的人口统计学和心血管危险因素外,乳腺癌分期与AF的发展密切相关[美国癌症联合委员会(AJCC)II/III/IV期与I期:调整后的风险比(aHR)分别为1.51/2.63/4.21]。乳腺癌诊断后新发AF(aHR为3.00)与1年心血管死亡率增加有关。
由此可见,女性确诊乳腺癌后AF发生率明显更高。诊断时较高的乳腺癌分期与较高的AF风险显著相关。在新的乳腺癌诊断中,新发AF会增加1年心血管死亡率,但不会增加与乳腺癌相关的死亡率。
原始出处:
Avirup Guha.et al.Incidence, risk factors, and mortality of atrial fibrillation in breast cancer: a SEER-Medicare analysis.European Heart Journal.2021.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehab745/6427396
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#发生率#
39
#ART#
35
#HEART#
33
#乳腺癌患者#
31
学习一下
159
好
155
学习了 赞
160
是否与治疗有关咧
169
学习了
156
房颤坚持抗凝很重要
26