Leuk Res:多西帕他钠 (DSTAT),一种 CXCL12/CXCR4 抑制剂,与阿扎胞苷联合用于治疗低甲基化剂难治性 AML 和 MDS
2022-01-17 MedSci原创 MedSci原创
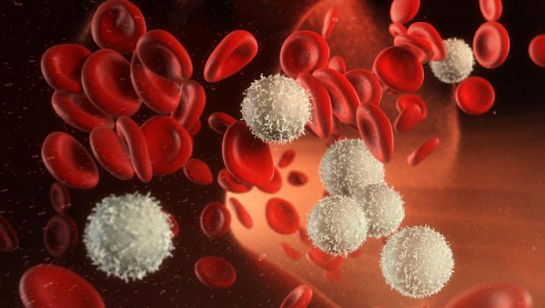
白血病干细胞利用细胞粘附分子(如 CXCR4/CXCL12)来归巢于骨髓基质微环境,在那里它们维持在休眠、受保护的状态。多西帕他钠 (DSTAT, CX-01) 是一种低抗凝肝素,具有多种作用机制,包
白血病干细胞利用细胞粘附分子(如 CXCR4/CXCL12)来归巢于骨髓基质微环境,在那里它们维持在休眠、受保护的状态。多西帕他钠 (DSTAT, CX-01) 是一种低抗凝肝素,具有多种作用机制,包括抑制 CXCR4/CXCL12 轴、阻断 HMGB1 和结合血小板因子 4 (PF-4)。
一研究团队进行了一项在阿扎胞苷中添加 DSTAT 的初步研究,用于对先前的低甲基化药物治疗无反应或复发的 AML 或 MDS 患者,假设 DSTAT 可能会提高反应率。招募了 20 名患者,中位值为 2 条先前的治疗线和 6 周期的先前低甲基化剂。
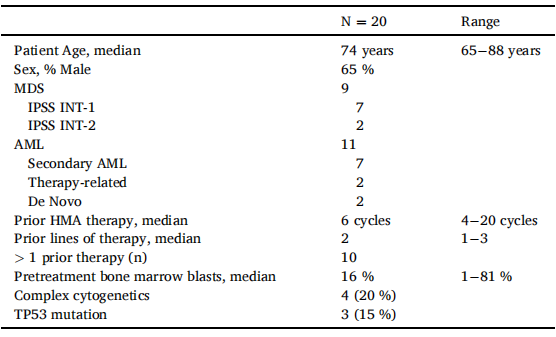
表1:患者和疾病的特征。

表2:在使用DSTAT和氮胞替丁治疗期间发生的III/IV级不良事件。
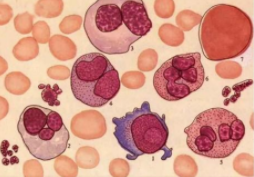
在可评估反应的 15 名患者中,有 1 名完全缓解,3 名骨髓完全缓解,可评估患者的反应率为 27%(总体为 20%)。在另外 5 名患者中观察到血液学改善。所有入组患者的中位总生存期为 205 天 (95 % CI 119–302)。虽然血细胞减少和感染很常见,但这些与仅接受阿扎胞苷治疗的患者人群的预期情况并没有不成比例。
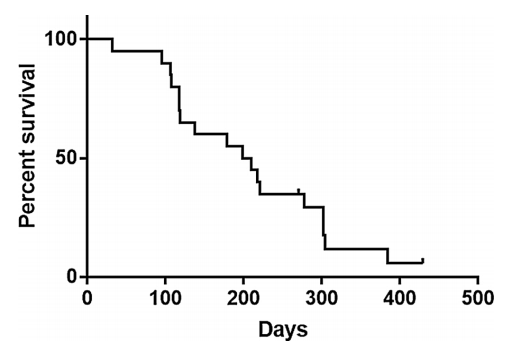
图1:所有使用DSTAT和氮胞苷治疗的患者的总生存期。
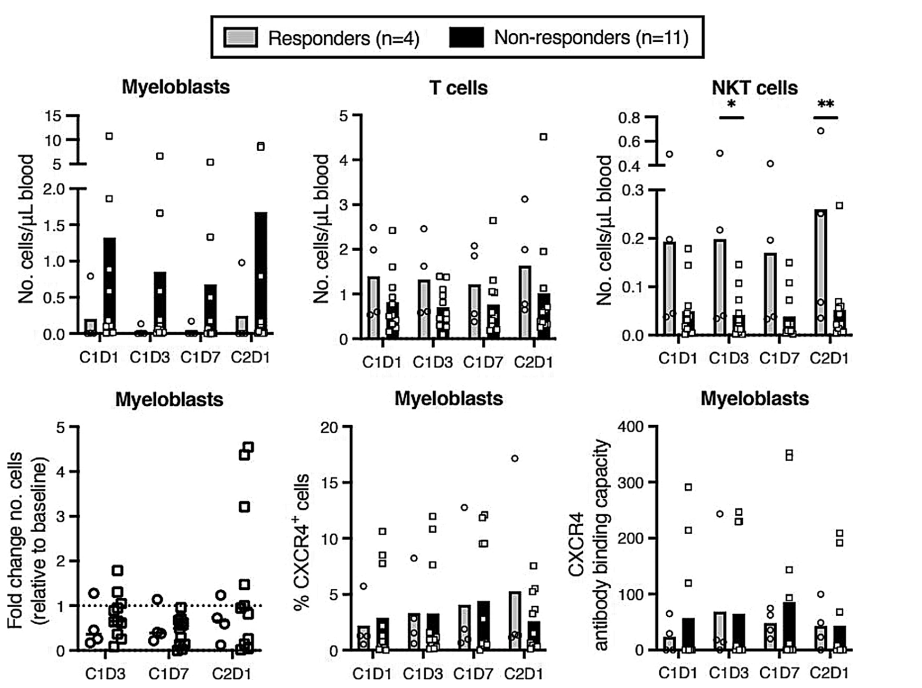
图2:对第1天1(C1D1)、C1D3、C1D7和C2D1进行荧光激活细胞分类,比较有反应者和无反应者(n=11),发现C1D3和C2D1循环NKT细胞的绝对数量略有增加(*表示p<0.05)。在使用DSTAT和氮胞苷治疗期间,在这些时间点上观察到成髓细胞动员或其他免疫细胞亚群没有显著差异。
总之,该试验证明了将 DSTAT 与阿扎胞苷联合使用的可行性,并观察到了几种反应,表明这种组合值得进一步研究。这些与仅接受阿扎胞苷治疗的患者群体的预期结果并不成比例。
原始出处:
Huselton E, Rettig MP, Campbell K, Cashen AF, DiPersio JF, Gao F, Jacoby MA, Pusic I, Romee R, Schroeder MA, Uy GL, Marcus S, Westervelt P. Combination of dociparstat sodium (DSTAT), a CXCL12/CXCR4 inhibitor, with azacitidine for the treatment of hypomethylating agent refractory AML and MDS. Leuk Res. 2021 Nov;110:106713. doi: 10.1016/j.leukres.2021.106713. Epub 2021 Sep 22. PMID: 34619434.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CXCL1#
50
#MDS#
50
#抑制剂#
54
!!!
102
#CXCR4#
49
#难治性#
43