
多发性硬化症(MS)是一种由环境因素引发的自身免疫性疾病,其作用于遗传上易感的宿主。多发性硬化症最不为人所知的方面之一是与复发-缓解型多发性硬化症(RRMS)向进展型多发性硬化症过渡有关的生物学因素。进展型多发性硬化症对治疗更难接受,与更大的身体残疾和生活质量损害有关,包括疲劳和抑郁。因此,迫切需要了解与进展性多发性硬化症有关的因素以及如何改变这些因素。
微生物群包括数万亿的生物体,它们可以通过调节从肠道到大脑的免疫细胞、分泌神经活性代谢产物、改变内分泌信号通路和触发传入神经元来影响神经系统疾病。动物模型的研究表明,肠道微生物群可以影响神经炎症。无菌和抗生素处理的小鼠对诱发和自发的实验性自身免疫性脑脊髓炎(EAE)(多发性硬化症的动物模型)都有抵抗力。给予促进T调节细胞的细菌,包括多糖A阳性的脆弱细菌,可以改善EAE,而给予诱导Th17细胞的细菌可以使EAE恶化。
此外,细菌可能通过生物模拟和炎症共同作用,诱发脊髓炎症。用来自RRMS患者的微生物群对自发EAE小鼠进行定植会使疾病恶化,并与产生IL-10的T regs减少有关。将MS微生物群与人类外周血单核细胞一起孵化,在体外诱发促炎症反应,表明MS微生物群既缺乏调节自身免疫力的有益微生物,又有过多的促炎症细菌。
一些实验室已经报道了RRMS的微生物群改变,包括阿克曼氏菌的增加和丁酸盐生产菌的减少。多发性硬化症中的微生物群改变可能是疾病的主要驱动因素,也可能反映了疾病过程中的次要改变。宿主可以通过分泌microRNAs来塑造微生物群。此外,MS患者和EAE高峰期的小鼠的肠道miR-30d升高,这增加了Akkermansia的水平并改善了EAE。这表明,Akkermansia的升高可能是积极的宿主选择的结果,而不是对MS的贡献。
研究发现,RRMS患者的普雷沃特氏菌水平较低,而施用人源普雷沃特氏菌可改善EAE,这表明增加耗损的细菌可减轻神经炎症。对RRMS患者施用益生菌可以逆转外周单核细胞的炎症表型,而且免疫变化在停止使用益生菌的几个月后仍然持久。总之,这些研究表明,微生物群在多发性硬化症中起着重要作用,调节微生物群具有治疗潜力。迄今为止,对进行性多发性硬化症的微生物群的研究很少。
藉此,哈佛大学的Laura M. Cox等人,探究了进展期多发性硬化症(MS)的肠道微生物组以及它与临床疾病的关系。
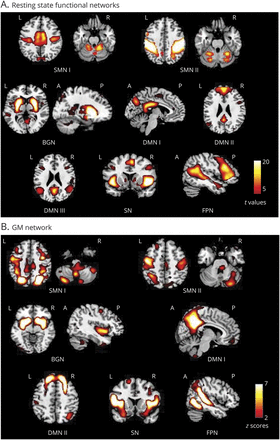
他们对健康对照组、复发性多发性硬化症(RRMS)和进展性多发性硬化症患者的微生物群进行了测序,并将细菌水平与疾病的临床特征相关联,包括扩展的残疾状态量表(EDSS)、生活质量和脑磁共振成像病变/萎缩。我们用MS衍生的Akkermansia定植小鼠,并诱发实验性自身免疫性脑脊髓炎(EAE)。
他们发现,微生物群的β-多样性在多发性硬化症患者和对照组之间存在差异,但在RRMS和进展性MS之间没有差异,也没有基于疾病修饰疗法的差异。
疾病状态对微生物群β-多样性的影响最大,其次是身体质量指数、种族和性别。在进行性多发性硬化症和RRMS中,Bolteae梭菌、Ruthenibacterium lactatiformans和Akkermansia增加,Blautia wexlerae、Dorea formicigenerans和Erysipelotrichaceae CCMM减少。在进行性多发性硬化症中,我们发现肠杆菌科和梭状芽孢杆菌g24 FCEY升高,Blautia和Agathobaculum下降。
。一些梭菌类与较高的EDSS和疲劳评分有关。与认为多发性硬化症患者的阿克曼氏菌升高有不利作用的观点相反。阿克曼氏菌与较低的残疾率有关,表明其有有益作用。
另外,从MS患者体内分离出的Akkermansia能改善EAE,这与RORγt+和产生IL-17的γδ T细胞的减少有关。
这个研究的重要意义在于:虽然一些微生物群的改变在复发性和进展性多发性硬化症中是共同的,但发现了与进展性多发性硬化症和疾病的临床措施有关的独特细菌。此外,多发性硬化症中阿克曼西亚的升高可能是多发性硬化症微生物群中的一种补偿性有益反应。
原文出处:
Cox LM, Maghzi AH, Liu S, Tankou SK, Dhang FH, Willocq V, Song A, Wasén C, Tauhid S, Chu R, Anderson MC, De Jager PL, Polgar-Turcsanyi M, Healy BC, Glanz BI, Bakshi R, Chitnis T, Weiner HL. Gut Microbiome in Progressive Multiple Sclerosis. Ann Neurol. 2021 Jun;89(6):1195-1211. doi: 10.1002/ana.26084. Epub 2021 Apr 30. PMID: 33876477; PMCID: PMC8132291.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Neurol#
27
#多发性#
33
#硬化症#
24
#肠道菌#
36
肠道菌群越来越重要
45
nice
55
学习学习
55
不错
60
看看
52
好文章,谢谢分享。
28