Science Advances:通过水凝胶递送CAR-T细胞,改善实体瘤治疗效果
2022-04-10 nagashi “生物世界”公众号
自2017年以来,全球共有7款CAR-T疗法获批上市,我国也上市了两款CAR-T疗法,然而,这些CAR-T疗法都是治疗血液类肿瘤。在治疗实体瘤方面,CAR-T仍未获得实质性突破。
近年来,肿瘤免疫疗法的兴起为广大癌症患者带来了新的希望,其中,CAR-T细胞疗法无疑是受关注的。简单来说,这种癌症疗法就是收集癌症患者的T细胞并对其进行重新编程,然后再把它们输送回患者体内,这些改造后的CAR-T细胞就会精准地摧毁癌细胞,让癌症患者重获新生。
自2017年以来,全球共有7款CAR-T疗法获批上市,我国也上市了两款CAR-T疗法,然而,这些CAR-T疗法都是治疗血液类肿瘤。在治疗实体瘤方面,CAR-T仍未获得实质性突破。
2022年4月8日,斯坦福大学的研究人员在 Science Advances 期刊发表了题为:Delivery of CAR-T cells in a transient injectable stimulatory hydrogel niche improves treatment of solid tumors 的研究论文。
该研究开发了一种简单而高效的CAR-T递送方法:将CAR-T细胞和细胞因子添加到特制水凝胶中,这种水凝胶在体内提供了一个临时的、可以激活免疫细胞的环境,然后泵出激活的CAR-T细胞攻击肿瘤组织。
更重要的是,这种递送方法具有治疗远端肿瘤的潜力,这为CAR-T治疗实体瘤打开了新的大门。
该研究的通讯作者、斯坦福大学助理教授 Eric Appel 博士表示:“很多CAR-T研究在关注如何做出更好的细胞,但少有研究关注如何让CAR-T细胞更有效地在体内发挥效用,而我们的这项研究是很好的补充。”
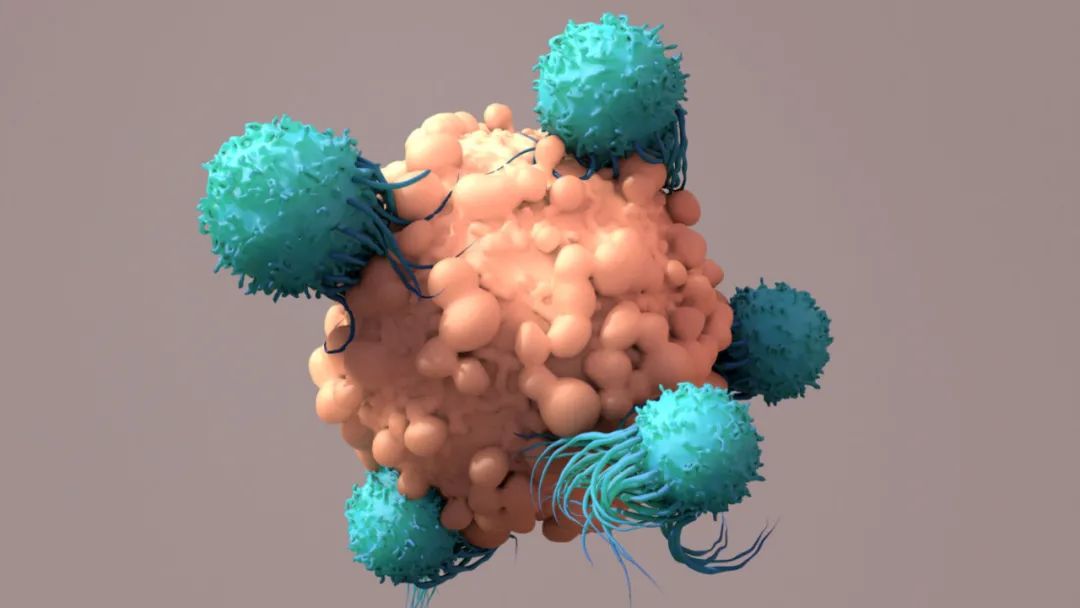
目前,静脉注射是CAR-T细胞治疗的主要方式。在这种方法中,CAR-T细胞会进入血液并流经全身,因而对血液癌效果十分显着。但这种方法对于治疗实体肿瘤并不理想,实体瘤通常很致密,存在于特定部位,并且有防御机制来隐藏自身或抵御免疫细胞的攻击。
打个形象的比喻,血液癌就像是孤立无援的散兵游将,因此更容易被击溃,但实体瘤就像是躲在城池中的部队,显然更为“根深蒂固”,CAR-T细胞很难渗透到实体瘤中去攻击癌细胞。
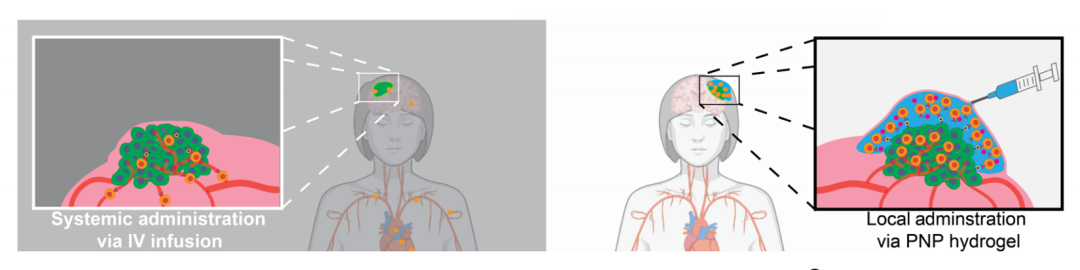
“水凝胶疗法”(右)和常规静脉注射(左)的区别示意图
为了强有力地激活CAR-T细胞,这些细胞必须长时间暴露在高浓度的特化信号蛋白中,这些蛋白质被称为细胞因子,它们会促进被改造的免疫细胞快速复制并准备摧毁肿瘤。然而,如果通过静脉注射输送,发动有效攻击所需的细胞因子数量将会对体的其他部分产生毒性。
因此,为了克服这个困难,研究团队创造了一种特殊的水凝胶,它附着在肿瘤组织周围,并可以暂时容纳细胞因子和CAR-T细胞,免疫细胞在那里生长和增殖,然后不断“泵出”CAR-T细胞杀死癌细胞。
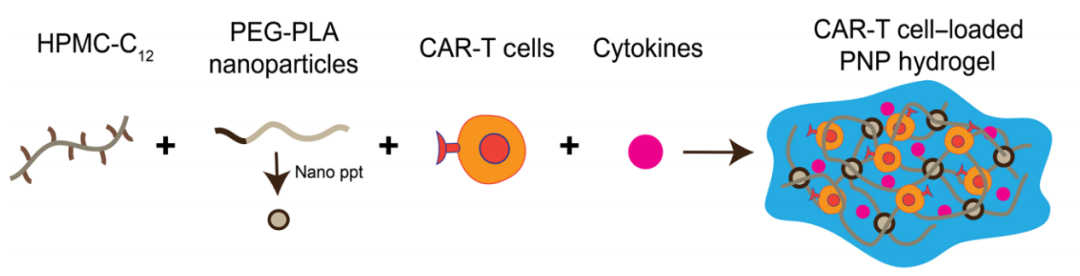
水凝胶的制备模式图
这种水凝胶由水和两种成分组成:一种是由植物中发现的纤维素制成的聚合物,另一种是可生物降解的纳米颗粒。当两者结合在一起时,就像魔术贴一样,它们可以粘在一起,也很容易被分开。
该研究的第一作者 Abigail Grosskopf 博士表示:“这种材料可以通过小针头注射,但在注入后,‘魔术贴’会发挥作用并转变成一个坚固的凝胶结构。凝胶的网状结构编织得足够紧密,以防止微小的细胞因子泄露,与此同时,这个结构的连接也非常脆弱,激活的CAR-T细胞可以将其破坏,进而将CAR-T细胞释放出去杀伤癌细胞”
在确定了提供癌症治疗的最佳水凝胶配方后,研究团队将其方法应用于患有肿瘤的小鼠身上。他们发现,所有的实验小鼠在注射了同时含有CAR-T细胞和细胞因子的水凝胶后,12天后肿瘤消失了。与之相对,只含有CAR-T细胞的实验组,小鼠的肿瘤消失得更慢甚至根本没有消失。
不仅如此,研究团队还尝试在离肿瘤较远的地方注射水凝胶,以验证该疗法是否可以治疗远端肿瘤。令所有人惊讶的是,即使注射部位在肿瘤生长的另一侧,所有小鼠的肿瘤仍然消失了,但治疗所需的时间是注射在肿瘤附近部位的两倍。
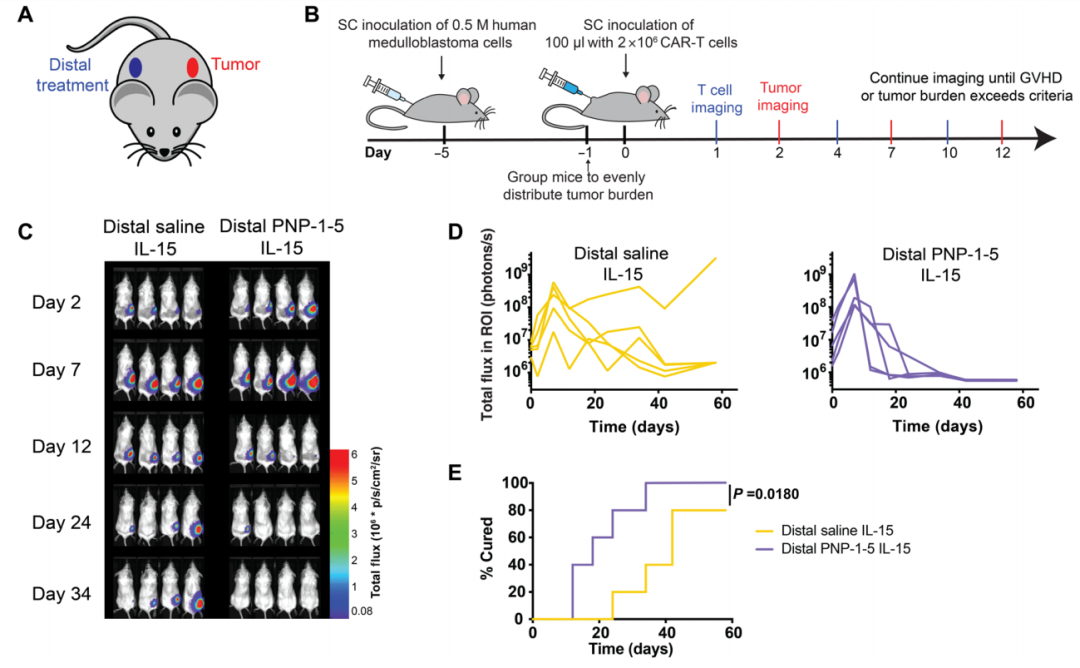
水凝胶对治疗小鼠远端皮下髓母细胞瘤有效
通讯作者 Eric Appel 博士表示:“在一些情况下,肿瘤可能在患者身体的深处,我们无法直接注射到肿瘤附近,而这种‘水凝胶疗法’表现出治疗远端肿瘤从强大潜力,在远离肿瘤的地方进行注射并发挥治疗作用的能力,为治疗各种实体肿瘤打开了大门。”
至于安全性方面,水凝胶在小鼠中没有引起不良炎症反应,并且在几周内就在体内完全降解了。
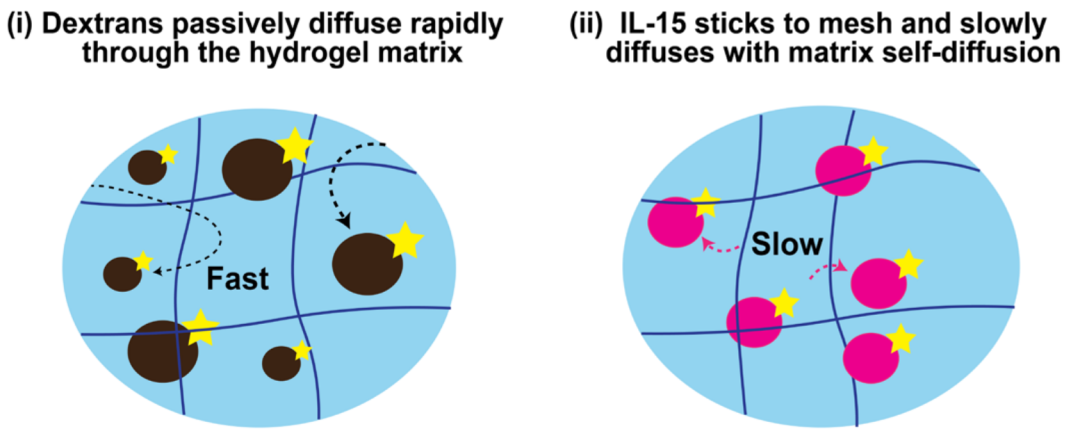
水凝胶可以延长刺激细胞因子的保留时间,并在体内表现出可控的降解
总的来说,该研究开发了一种简单而高效CAR-T细胞递送方法——通过特制的水凝胶包裹CAR-T细胞和细胞因子,水凝胶会在实体瘤部位不断“泵出”激活的CAR-T细胞,迅速清除肿瘤。
更重要的是,这种递送方法具有治疗远端肿瘤的潜力,这为CAR-T治疗实体瘤打开了新的大门,也为人类彻底攻克癌症指明了新的方向。此外,水凝胶递送的方法还有一大好处,就是制备简单,从而有助于简化流程,降低CAR-T疗法成本和价格。
原始出处:
ABIGAIL K. GROSSKOPF, et al. Delivery of CAR-T cells in a transient injectable stimulatory hydrogel niche improves treatment of solid tumors. SCIENCE ADVANCES, 8 Apr 2022, Vol 8, Issue 14 ? DOI: 10.1126/sciadv.abn8264.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CAR-#
51
#治疗效果#
35
#水凝胶#
0
#SCIE#
39
#凝胶#
47