BMC Cancer:倾向评分匹配(PSM)研究表明抗PD-1联合索拉非尼较抗PD-1单药改善晚期肝细胞癌患者的预后
2022-01-15 yd2015 MedSci原创
该研究首次表明,抗PD-1联合索拉非尼较抗PD-1单药改善晚期肝细胞癌患者的预后。
血管内皮生长因子(VEGF)在肿瘤微环境中发挥作用。索拉非尼抑制VEGF通路,具有免疫调节功能,但缺乏大量临床数据。因此,来自我国台北学者开展了一项倾向评分匹配(PSM)研究,旨在探讨抗PD - 1联合索拉非尼治疗晚期肝细胞癌的疗效。相关结果发表在BMC Cancer杂志上。
我们回顾了2016年1月至2019年2月在台北荣民总医院(台北)接受抗PD - 1治疗的HCC患者。进行倾向性评分匹配后,比较两组疗效。
筛查173例患者,最终纳入140例HCC患者,58例联合使用抗pd -1和索拉非尼,82例单独使用抗pd -1,中位随访时间为9.1个月。Nivolumab治疗123例(87.9%),而pembrolizumab治疗17例(12.1%)。匹配前,联合组ALBI评分显著高于对照组,PVT显著高于对照组(74.1% vs. 46.3%,p<0.05)和更晚期的BCLC期(C期94.8% vs. 81.7%, p<0.05)。
与单独抗pd -1相比,联合治疗有更高的CR率(8.6% vs. 4.9%, n.s .)、ORR (22.4% vs. 19.5%, n.s .)和更高的DCR (69.0% vs. 37.8%, p<0.05)。配对后,联合治疗的DCR仍然较高。
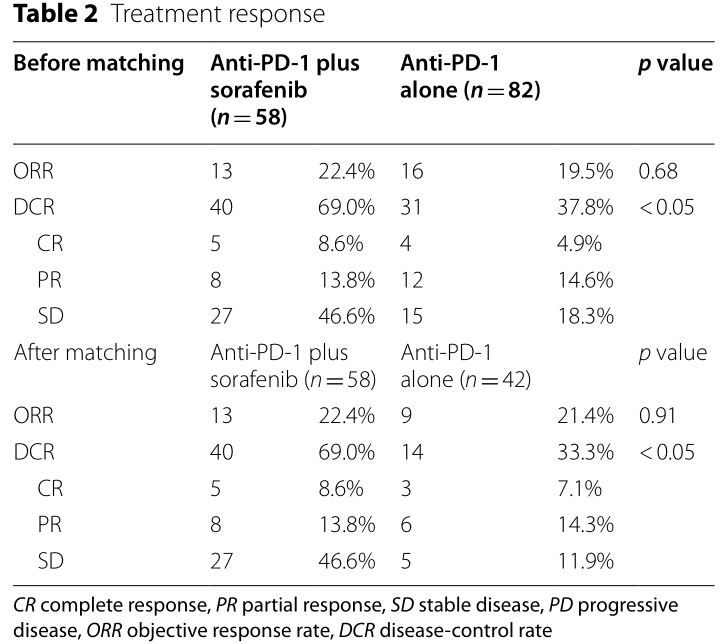
PSM前后疗效评估
配对后,联合组获得更长的无进展生存期(3.87 vs. 2.43个月,HR 0.62, [0.38–1.00],p<0.05)和总生存期(未达到vs. 7.17个月,HR 0.62, [0.38–1.00],p<0.05)。
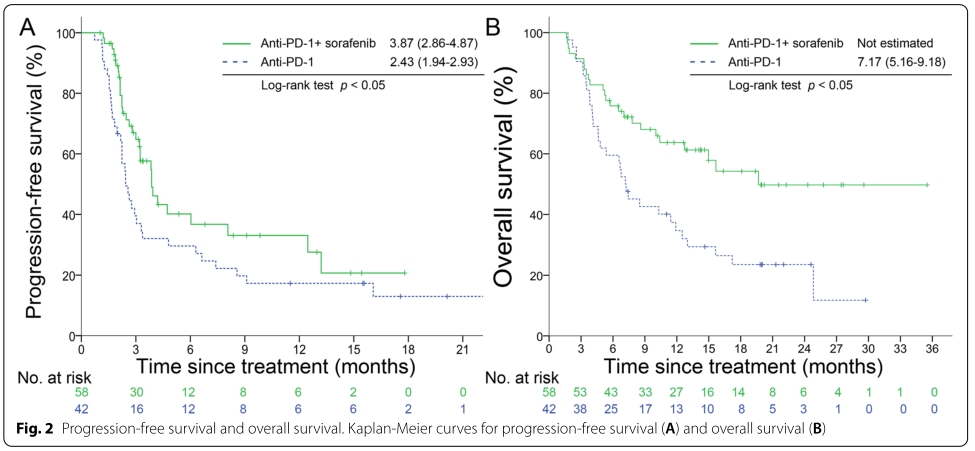
PSM后PFS和OS
亚组分析也发现联合治疗较抗PD-1单药治疗改善大多数亚组的PFS和OS。
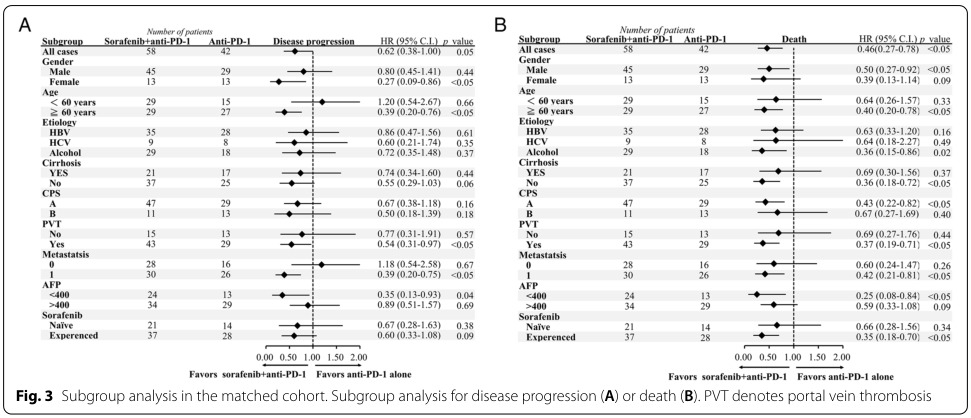
亚组分析
AFP的下降与治疗的CR率和ORR相关,下降越多,联合治疗组的CR率和ORR越高。
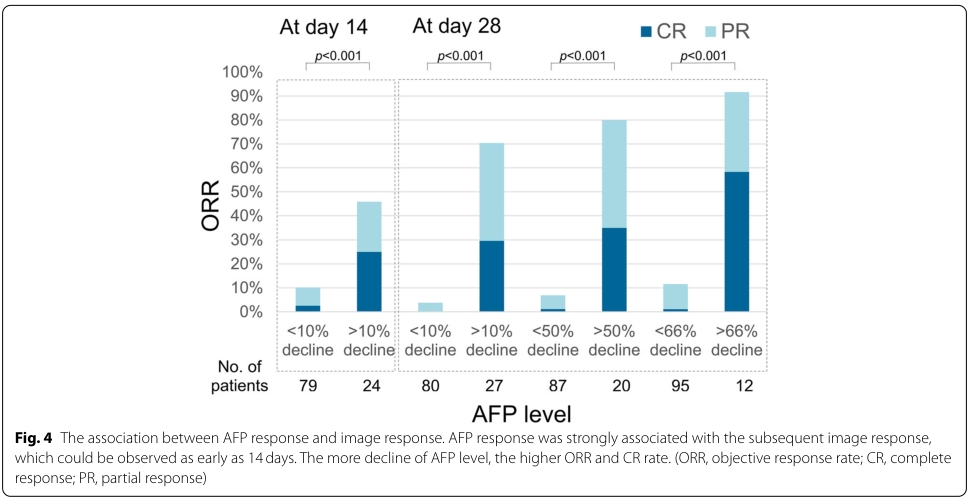
AFP变化与疗效关系
综上,该研究首次表明,抗PD-1联合索拉非尼较抗PD-1单药改善晚期肝细胞癌患者的预后。
原始出处:
Chen SC, Huang YH, Chen MH, Hung YP, Lee RC, Shao YY, Chao Y. Anti-PD-1 combined sorafenib versus anti-PD-1 alone in the treatment of advanced hepatocellular cell carcinoma: a propensity score-matching study. BMC Cancer. 2022 Jan 11;22(1):55. doi: 10.1186/s12885-022-09173-4. PMID: 35016637.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肝细胞#
43
#倾向评分匹配#
29
#细胞癌#
39
#BMC#
34
#晚期肝细胞癌#
34