ESMO:帕博利珠单抗降低完全切除、早期非小细胞肺癌24%复发或死亡风险(KEYNOTE-091)
2022-03-26 网络 网络
3月17日,ESMO Virtual Plenary Resources发布了PEARLS/KEYNOTE-091 (NCT02504372) 研究结果。研究评估了帕博利珠单抗作为辅助治疗在完全切除的
3月17日,ESMO Virtual Plenary Resources发布了PEARLS/KEYNOTE-091 (NCT02504372) 研究结果。研究评估了帕博利珠单抗作为辅助治疗在完全切除的早期非小细胞肺癌(NSCLC) 患者中的疗效。
KEYNOTE-091研究同样使用了AJCC 第7 版肺癌分期系统,不过术后的含铂辅助治疗不是必要项,研究纳入R0、IB期(T≥ 4 cm,II期或IIIA期NSCLC),1:1随机分至帕博利珠单抗组或安慰剂组。

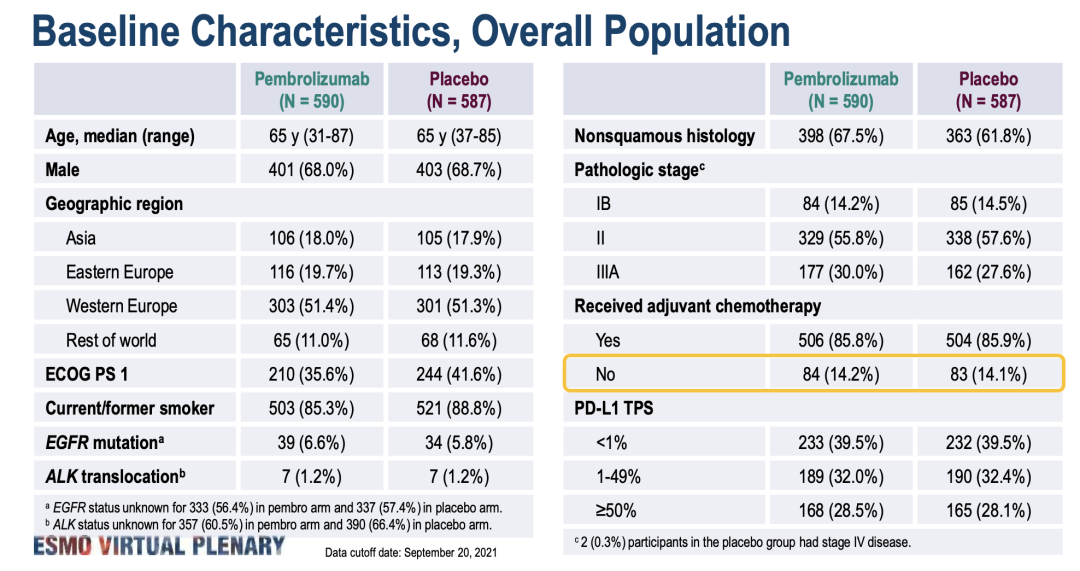
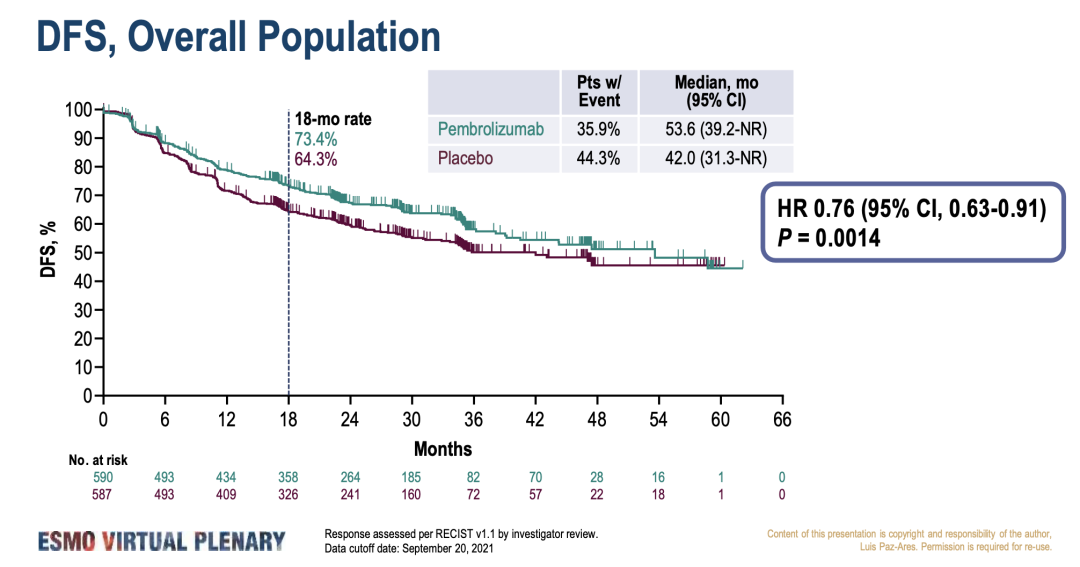
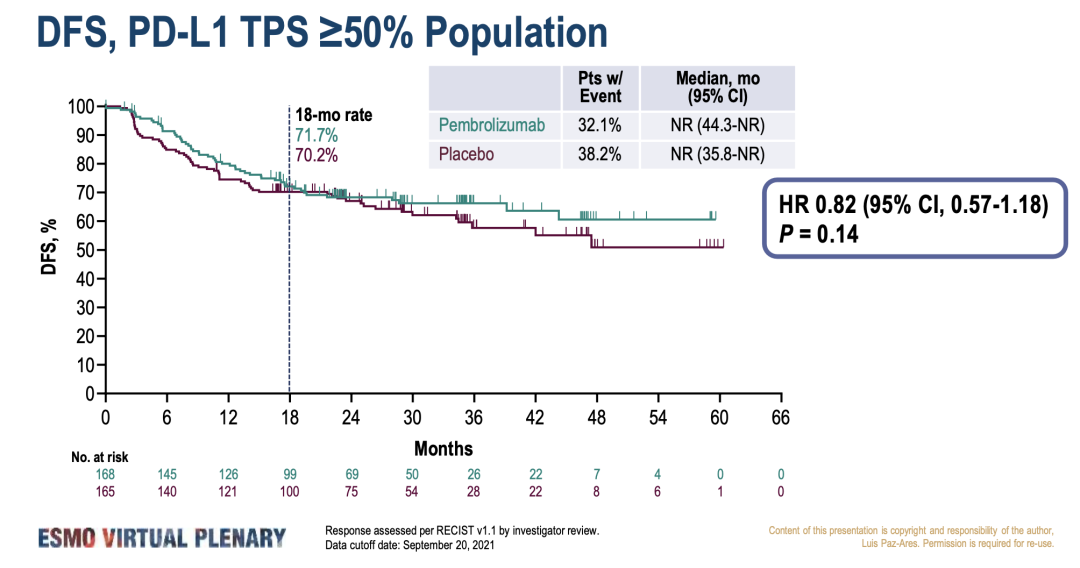
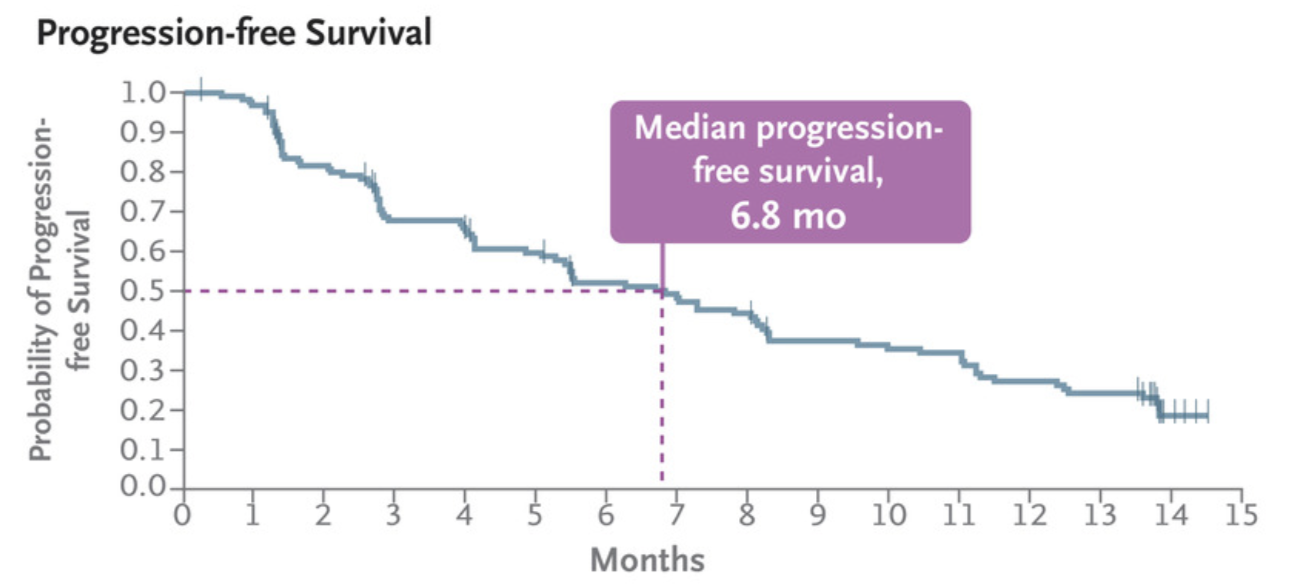
组间基线特征平衡。全人群中,帕博利珠单抗显著改善了 DFS(53.6个月 vs 42.0 个月;HR 0.76;95% CI 0.63-0.91;P = 0.0014);TPS ≥ 50% 的人群中HR=0.82(95% CI 0.57-1.18;P = 0.14),曲线在18个月时出现交叉。
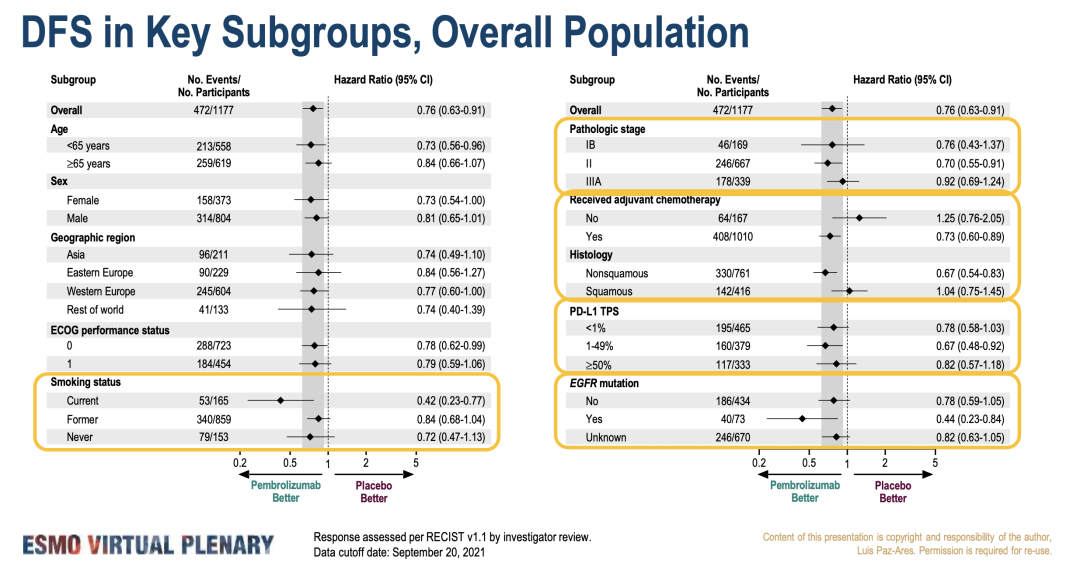
亚组分析中可以看到,接受过辅助化疗与没有接受过化疗人群的HR分别为0.73与1.25,提示术后辅助化疗的重要性。
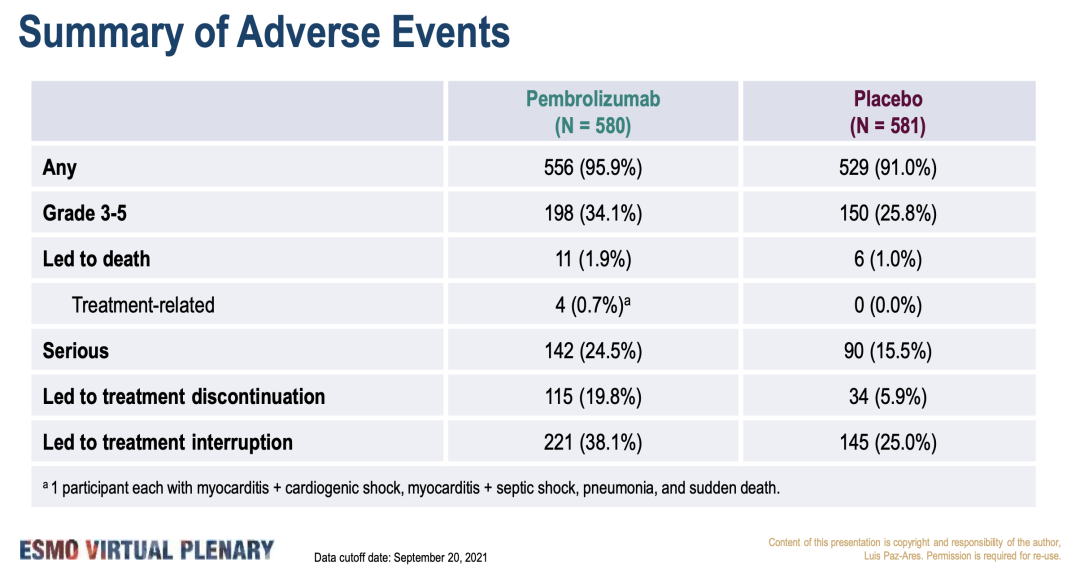
研究中帕博利珠单抗的安全性如预期。
结论:无论 PD-L1 表达如何,帕博利珠单抗辅助治疗为完全切除的 IB 期 (T ≥ 4 cm)-IIIA NSCLC 患者(无论PD-L1 TPS <1%、1-49%、 ≥50%)提供了统计学上显著、具临床意义的 DFS 改善。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#非小细胞#
42
#SMO#
40
#帕博利珠单抗#与#NSCLC#
91
我觉得要和标准术后辅助方案比才有说服力,和安慰剂比不够给力
0
#帕博利珠#
44
#KEYNOTE#
42
#死亡风险#
35
#ESMO#
43
学习!
54