Stroke:老年脑出血主要病因——遗传性CAA磁共振标志物和认知能力的纵向发展情况
2022-04-05 网络 网络
淀粉样脑血管病(CAA)是老年人自发性脑出血的主要原因之一。
淀粉样脑血管病(CAA)是老年人自发性脑出血的主要原因之一,多数患者因脑出血入院,而CAA相关脑出血复发率高,所以根据Boston诊断标准,通过影像检查进行早期诊断对患者预后尤为重要。
CAA主要影像表现有脑叶出血、脑微出血、大脑凸面蛛网膜下腔出血及脑表面铁沉积,临床可常规运用磁敏感加权成像序列以增加CAA病灶的检出率。其中,β淀粉样蛋白(Aβ)沉积于皮质及软脑膜血管为CAA主要的病理特征。
目前认为出血性和缺血性磁共振成像病变以及最近描述的血管运动反应性下降被认为可能是CAA的生物标志物。对这些标志物的分析主要是在疾病的症状期的横断面,很少有关于其纵向发展的数据,特别是在疾病的症状前阶段,当它可能对治疗最有反应。

为此,来自荷兰莱登大学的学者利用研究荷兰型遗传性脑淀粉样血管病(D-CAA)提供的独特机会,确定CAA生物标志物在疾病的症状前和症状期的纵向发展规律,结果发表在stroke杂志上。
在这项纵向病例对照研究中,在基线和4年后对10名无症状和6名有症状的D-CAA突变携带者和20名对照受试者的磁共振成像标志物和认知能力进行评估。这些磁共振成像标志物包括出血性和缺血性表现,脑血流的测量,以及对视觉刺激的血管运动反应性。
结果显示,在无症状的D-CAA突变携带者中,血管运动反应性显示血氧水平依赖的振幅随时间下降(P=0.011),达到峰值的时间延长(P<0.001)。相比之下,出血性标志物、缺血性标志物、脑血流和认知能力没有发现明显变化。在有症状的D-CAA突变携带者中,脑内出血的数量在4年内有所增加(P=0.007)。
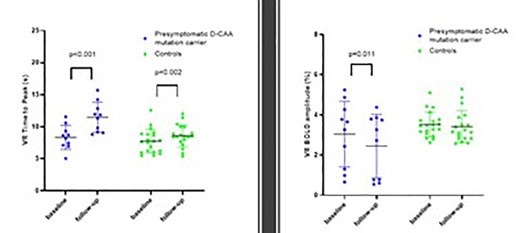
无症状D-caa携带者血氧水平以来的振幅变化
该研究结果表明,在D-CAA的无症状阶段,由血氧水平依赖性振幅和对视觉刺激达到峰值的时间测量的脑血管反应性逐渐恶化,因此可被视为疾病进展的标志。在有症状的阶段,最突出的进展标志似乎是复发的脑内出血。
参考文献:
Longitudinal Progression of Magnetic Resonance Imaging Markers and Cognition in Dutch-Type Hereditary Cerebral Amyloid Angiopathy. Stroke. 2022;0:10.1161/STROKEAHA.121.035826.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#遗传性#
38
#标志物#
43
#磁共振#
40
#CAA#
54