最近提出的一个机制是,由于与tau缠结(AD的病理特征之一)相关的促醒神经元和神经递质损失导致唤醒不足,从而造成睡眠-觉醒障碍和更高的日间午睡倾向。 反过来说,白天的过度困倦,可能是导致更长时间和频繁午睡的原因,也与认知能力下降或AD病理积累的速度有关。
然而,在之前的研究中,关于白天小睡对认知的影响仍然存在矛盾的结果。虽然一些研究显示小睡对急性认知表现、情绪和警觉性有好处,尤其是在年轻的成年人中,但更多的小睡也与长期的不良结果有关,包括认知能力差。 例如,一些横断面研究报告了自我报告的过度午睡与认知功能恶化之间的关联;最近的一项纵向研究也显示,在老年男性中,较长的午睡时间与较快的认知衰退之间存在关联。然而,其他研究也证明了相反的情况--自我报告的午睡与较低的认知障碍几率有关。
然而,所有先前的研究都只对每个参与者进行了一次午睡评估。目前仍不清楚白天的午睡是如何随着年龄的增长,特别是认知的衰老而演变的。此外,这些研究大多采用主观的午睡评估,可能并不可靠,特别是在老年人的认知状态下。要了解白天的午睡和AD之间的复杂联系,需要对客观午睡进行纵向评估。
藉此, 哈佛大学的Peng Li等人, 探究了:
(1)随着年龄的增长,参与者的午睡时间更长和/或更频繁,这种纵向变化随着参与者从无认知障碍到轻度认知障碍(MCI)的进展而加剧,并在诊断为阿尔茨海默氏痴呆后进一步加速;
(2)白天客观午睡时间过长(即更长和/或更频繁)的参与者患阿尔茨海默氏痴呆的风险增加。
他们发现:随着年龄的增长,老年人倾向于更长时间和更频繁地午睡,而阿尔茨海默氏症的进展加速了这种变化,使每年的午睡时间/频率增加了一倍以上。
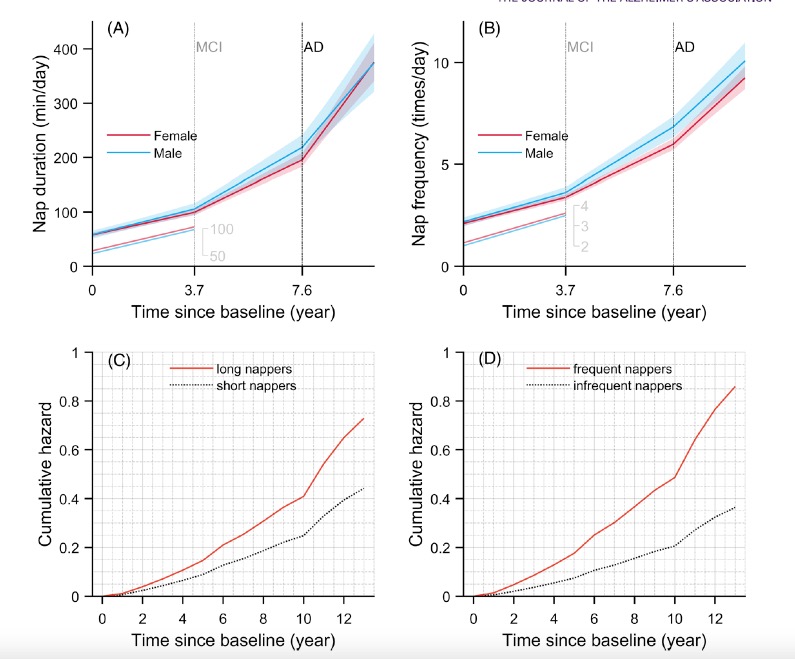
更长和更频繁的日间小睡与阿尔茨海默氏痴呆症的高风险有关。
有趣的是,更多过度(更长或更频繁)的日间小睡与一年后的认知能力更差相关,反之,更差的认知能力与一年后更多的过度小睡相关。
该研究的重要意义在于发现了:白天过度的午睡和阿尔茨海默氏症可能具有双向关系,或有共同的病理生理机制。
原文出处:
Li P, Gao L, Yu L, et al. Daytime napping and Alzheimer’s dementia: A potential bidirectional relationship. Alzheimer’s & Dementia. Published online March 17, 2022:alz.12636. doi:10.1002/alz.12636
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#dementia#
55
#ERS#
39
#alzheimers#
48
#MERS#
41
老年性痴呆,未来还是希望借助神经电生理吧,也许更为有效!
55