Diabetologia:HNF4A-MODY患者出生体重与糖尿病外显率的相关性
2021-11-12 从医路漫漫 MedSci原创
编码肝细胞核因子-4α的HNF4α突变可导致青年发病成年型糖尿病(MODY)。
编码肝细胞核因子-4α的HNF4α突变可导致青年发病成年型糖尿病(MODY)。HNF4A-MODY还与先天性高胰岛素血症(CHI)和新生儿低血糖有关。我们对从高胰岛素症向糖尿病的转变的理解有限。一种假设是,胎儿胰岛素分泌增加会触发细胞凋亡,并导致出生后β细胞加速衰竭。或者,HNF4A缺乏会在生命的早期和晚期引起明显的转录缺陷,导致胰岛素表型的反差。这两种假设对于子宫内胰岛素分泌过多是否会在以后的生活中导致β细胞衰竭有所不同。
众所周知,人类中胎儿的胰岛素分泌水平是出生体重的主要决定因素。对胰岛素基因突变或胰腺发育不全导致胎儿胰岛素分泌完全缺失的个体进行了分析,结果显示,这些个体的出生体重为正常出生体重的一半。此外,据报道,在HNF4A突变个体中,新生巨大儿常发生高胰岛素血症低血糖。因此,出生体重可能是胎儿预测胰岛素分泌的有用指标。在这项研究中,我们试图确定HNF4A突变个体的出生体重和糖尿病外显率之间的关系,这可以为胎儿和成人胰岛素分泌能力之间的关系提供见解。
从基因测试转录表中提取了所有出生体重数据和罕见致病HNF4A突变的个人的数据。由于缺乏群体水平的测序数据,这是确定变异外显性和致病性所必需的,因此我们排除了一小部分自我报告为非白人的个体(n=7)。研究中年龄小于7岁的个体(n=63)也因缺乏糖尿病表现而被移除。最后,为了准确确定正确的出生体重,去除了一小部分自我报告为双胞胎的个体(n=4)或妊娠32周的双胞胎或≤个体(n=3)。这导致了这里给出的队列(n=186,临床特征见电子补充材料表1)。我们队列的特征意味着我们计算出我们有>80%的能力来检测HR≥1.43或≤0.70。使用儿童成长基金会参考标准将儿童体重指数调整为成人等值。出生体重根据英国1990/UK-WHO生长标准进行了孕期和性别校正,并使用ZARONO软件包进行了计算。使用Stata v16进行统计分析。这项研究得到了北威尔士研究伦理委员会(17/WA/0327)和莫托大学医院伦理委员会的伦理批准。
我们首先试图评估母亲糖尿病病史和HNF4A突变对新生儿体重的影响。有突变个体的出生体重高于无突变家庭成员(4.17 kg[IQR=3.6~4.71],n=186vs3.66 kg[IQR=3.3~4.18],n=31;P<0.001)。当分析限于未报告患有糖尿病的母亲所生的个体(4.03kg[IQR=3.64-4.56],n=72VS3.44kg[IQR=3.2 4-3.85],n=20;p=0.001)时,结果是相似的。(图1a)。此外,对于携带突变的个体来说,那些怀孕期间患有糖尿病的母亲所生的婴儿比那些从未报告患有糖尿病的母亲所生的婴儿的出生体重更高(4.47 kg[IQR=3.76-4.88],n=55vs4.03 kg[IQR=3.64-4.56],n=72;p=0.04)(F i.g.1a)。
为了评估出生体重对外显性的影响,我们进行了单变量COX比例风险生存分析,发现每公斤体重增加与糖尿病诊断率下降22%相关(HR=0.78[95%CI=0.62,0.97];p=0.03)(表1)。对于出生体重低于4.17公斤(队列中位数)的人,50%的人在22岁时患上糖尿病,而对于出生体重超过4.17公斤的人,50%的人通过30年出生体重(图1b)患上糖尿病。当分析仅限于具有蛋白质截断变异的个体(HR=0.64,95%CI=0.42,0.98,p=0.04)或可能的父系遗传突变(父亲报告患有糖尿病和/或突变,母亲报告没有糖尿病)时,我们观察到类似的结果(HR=0.63,95%CI=0.40,0.99,p=0.0 5)
为了评估出生体重是否与外显性独立相关,我们进行了多变量COX比例风险生存分析,调整了其他影响外显性的因素。为了确定与HNF4A-MODY外显性相关的因素,我们比较了20岁时糖尿病患者和非糖尿病患者的特征(队列中糖尿病诊断的中位年龄)。除了出生体重较低外,女性以及母亲在怀孕期间所生的糖尿病与较早发病有关(均<0.05)(表1)。调整这些变量后,出生体重对外显性的影响仍然是独立的,每公斤体重每增加一次,糖尿病诊断减少30%(HR=0.70[95%CI=0.54,0.91];p=0.008,表1)。
我们发现,在具有高穿透性HNF4突变的个体中,出生体重较高与糖尿病外显性降低有关。我们推测,这反映了个体胎儿和成人胰岛素分泌能力之间的相关性,即携带HNF4A突变和出生体重较高的个体成年β细胞功能下降较少。对围产期血糖/胰岛素水平的直接测量和对β细胞功能的纵向研究可以得出更可靠的结论,但这些研究本身就很困难,而且成本高昂。
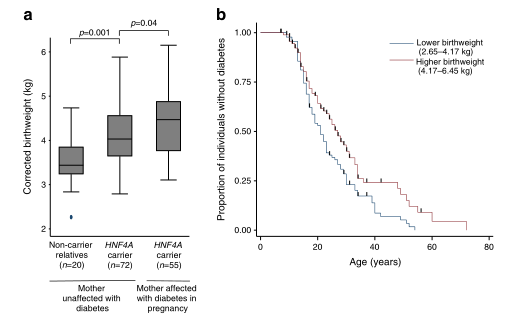
HNF4基因突变与出生体重的增加不依赖葡萄糖有关,而较高的出生体重与对糖尿病的相对保护有关。(A)HNF4基因突变个体的性别和妊娠校正出生体重(按孕期是否患有糖尿病划分)和非携带者亲属的p值由Mann-WhitneyUtest计算。每个框内的水平线表示中间值,框的顶部和底部分别表示第75个百分位数和第25个百分位数。胡须指示最大值和最小值,不包括异常值。实心圆圈表示异常值。(B)携带HNF4突变的个体从糖尿病中存活下来的Kaplan-Meier图(n=186)

表1 用Cox比例风险生存回归分析确定HNF4a-MODY外显性相关因素的危险比
总之,这是研究HNF4α-MODY外显率影响因素的第一个和最大的研究之一,确定了出生体重作为潜在预后和治疗相关指标的重要性。
原文出处:
Locke JM, Dusatkova P, Colclough K,et al.Association of birthweight and penetrance of diabetes in individuals with HNF4A-MODY: a cohort study.Diabetologia 2021 Oct 07
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BET#
40
#DIA#
34
#MODY#
38
#相关性#
32
#HNF4a#
49
#出生体重#
44
已拜读,受益匪浅。
58