Lancet Neurology:未破裂脑动静脉畸形(ARUBA)药物联合介入治疗与单纯药物治疗的比较:一项多中心、非盲、随机对照试验的最终随访
2020-11-28 MedSci原创 MedSci原创
一项未破裂的脑动静脉畸形(ARUBA)的随机试验中,在预先指定的中期分析中表明,在预防症状性中风或死亡方面,单纯的药物治疗优于药物治疗和介入治疗的联合治疗。
一项未破裂的脑动静脉畸形(ARUBA)的随机试验中,在预先指定的中期分析中表明,在预防症状性中风或死亡方面,单纯的药物治疗优于药物治疗和介入治疗的联合治疗,且其在平均33.3个月的随访中停止了随机试验。本文的目的是研究这些差异是否在5年的随访中持续存在。

方法:ARUBA是一项非盲随机试验,在9个国家的39个临床中心进行。其纳入标准为:成人(年龄≥18岁)被诊断为未破裂的脑动静脉畸形,从未接受过介入治疗,并且被参与的临床中心认为适合进行干预以根除病变。患者被一个基于网络的数据收集系统随机分配(1:1),由临床中心按照随机排列的区块设计分层,区块大小为2、4和6,单独进行药物治疗或联合介入治疗(单独或以任何组合、顺序或数量进行神经外科手术、栓塞或立体定向放射治疗)。虽然某个中心的病人和研究人员没有被隐瞒接受治疗任务,但其他中心的研究人员并没有被告知任何中心的任务或结果。主要结果是通过影像学证实的死亡时间或有症状的中风,由每个不参与参与者护理管理的中心的神经学家进行评估,并由一个独立的委员会使用适应性方法和中期分析进行监测。此项研究从2007年4月4日开始招募,2013年4月15日停止,之后继续跟进至2015年7月15日。
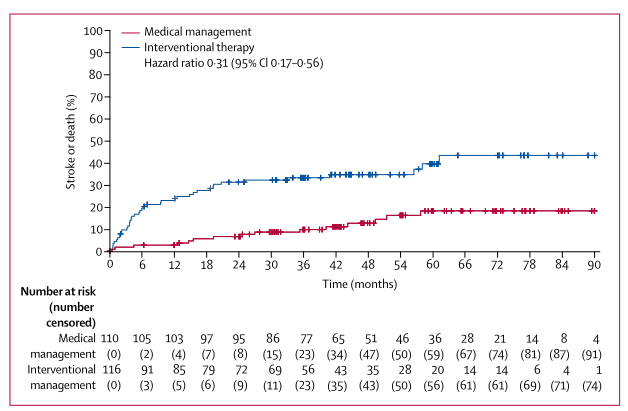
结果:在筛选出的1740名患者中,226名患者被随机分配到单独接受药物治疗(n=110)或药物联合介入治疗(n=116)。在平均50.4个月(标准差22.9)的随访中,单纯药物治疗的死亡或症状性中风的发生率(110例中15例,每100例病人年3.39例)低于介入治疗组(116例中41例,每100例病人年12.32;危险比0.31,95%可信区间0.17~0.56)。药物治疗组2例,介入治疗组4例(2例归因于介入治疗)在随访中死亡。与介入治疗相比,接受药物治疗的患者的不良事件发生率较低(283 vs 369;58.97 vs 78.73每100病患年;风险差异-19.76,95%CI-30.33-9.19)。
综上所述,经过平均50个月的随访,在ARUBA试验中,对于未破裂脑动静脉畸形患者的死亡或症状性卒中的预防,单独的药物治疗仍然优于药物联合介入治疗。
Mohr, Jay P et al. Medical management with interventional therapy versus medical management alone for unruptured brain arteriovenous malformations (ARUBA): final follow-up of a multicentre, non-blinded, randomised controlled trial. The Lancet Neurology, Volume 19, Issue 7, 573 - 581
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉#
39
#Neurol#
58
#对照#
57
#多中心#
48
#对照试验#
47
#动静脉畸形#
38
#药物联合#
51
#Lancet#
35
学习到了
100
#随机对照试验#
44