Ann Intern Med:SGLT2抑制剂 vs GLP-1 RA对有无CVD的T2D患者心血管事件风险的影响
2021-10-02 Nebula MedSci原创
与GLP-1 RA治疗相比,无论T2D患者是否合并心血管疾病,采用SGLT2抑制剂治疗均可明显降低心衰住院风险,其中合并心血管疾病的患者的绝对获益更明显
在关于2型糖尿病(T2D)和心血管疾病(CVD)的安慰剂对照试验中,钠-糖共转运体-2(SGLT2)抑制剂和胰高血糖素样肽-1受体激动剂(GLP-1 RA)均表现出了心血管方面的益处。
本研究旨在探究SGLT2抑制剂和GLP-1 RA是否与有无合并CVD的T2D患者的心血管获益差异有关。
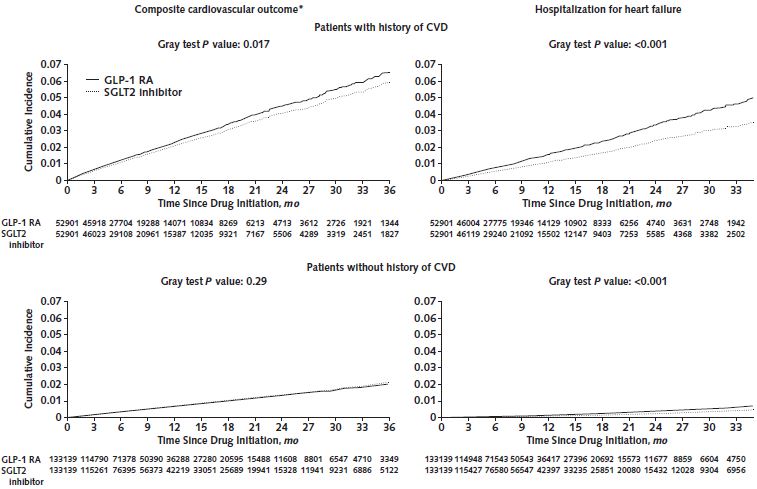
这是一项以人群为基础的队列研究,从美国医疗保险和商业保险数据库中1:1纳入采用SGLT2抑制剂或GLP-1 RA治疗的有无合并CVD的T2D患者(合并CVD的患者,n=52901;不合并CVD的患者,n=133139)。主要终点是心肌梗死(MI)或卒中住院和心衰住院(HHF)的复合终点。
GLP-1 RA vs SGLT2抑制剂对有无CVD的T2D患者的心血管事件风险的影响
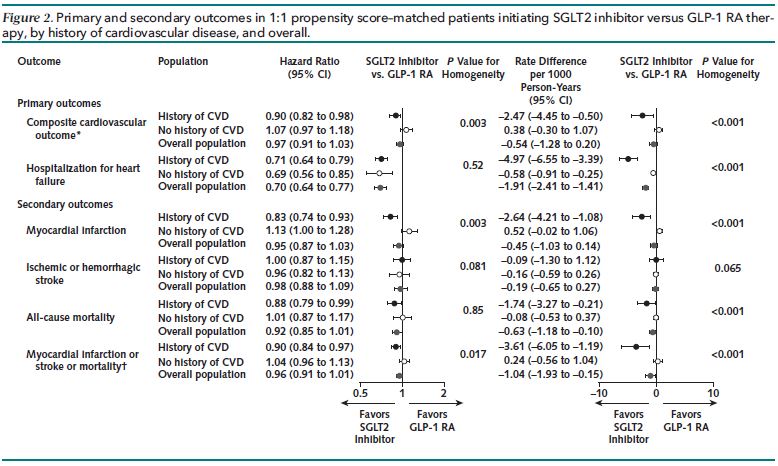
与GLP-1 RA治疗相比,SGLT2抑制剂治疗与合并心血管疾病的T2D患者的心肌梗死或卒中风险略微降低相关 (HR, 0.90 [95% CI, 0.82~0.98]; RD, -2.47 [CI, -4.45~-0.50]),但在不合并CVD的T2D患者中观察到相似的风险差异 (HR, 1.07 [CI, 0.97~1.18]; RD, 0.38 [CI, -0.30~1.07])。无论基线有无合并CVD,与GLP-1 RA治疗相比,启用SGLT2抑制剂治疗始终与受试患者的HHF风险降低相关(合并CVD:HR, 0.71 [CI, 0.64~0.79]; RD, -4.97 [CI, -6.55~-3.39];不合并CVD:HR, 0.69 [CI, 0.56~0.85]; RD, -0.58 [CI, -0.91~-0.25])。
各种次要终点事件的发生风险
综上所述,与GLP-1 RA治疗相比,无论T2D患者是否合并心血管疾病,采用SGLT2抑制剂治疗均可明显降低心衰住院风险,其中合并心血管疾病的患者的绝对获益更明显。GLP-1 RA和SGLT2抑制剂对有无合并心血管疾病的T2D患者的心肌梗死或卒中风险的影响无明显差异。
原始出处:
Patorno Elisabetta,Htoo Phyo T,Glynn Robert J et al. Sodium-Glucose Cotransporter-2 Inhibitors Versus Glucagon-like Peptide-1 Receptor Agonists and the Risk for Cardiovascular Outcomes in Routine Care Patients With Diabetes Across Categories of Cardiovascular Disease.[J] .Ann Intern Med, 2021, https://doi.org/10.7326/M21-0893
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血管事件#
33
#SGLT#
28
#2抑制剂#
38
#抑制剂#
33
#心血管事件风险#
43
#GLP-1#
35
#SGLT2#
33
#Med#
28