Lancet Gastroenterol Hepatol:非酒精性脂肪肝越严重,心血管事件风险越高!
2021-10-01 Nebula MedSci原创
NAFLD 与致命或非致命性 CVD 事件的长期风险增加有关
既往很多研究显示,非酒精性脂肪肝 (NAFLD) 与心血管疾病 (CVD) 发病率增加之间存在显著关联。但是,风险的大小以及这种风险是否随着 NAFLD 的严重程度而变化尚不确定。
Alessandro等研究人员对观察性研究进行了荟萃分析,以量化 NAFLD 与 CVD 事件风险之间的关联程度,研究结果于近日发表在柳叶刀子刊《Lancet Gastroenterol Hepatol》上。
研究人员系统地检索了 PubMed、Scopus 和 Web of Science 数据库 2021年7月1日前收录的研究,筛选评估 NAFLD 成年患者(≥18岁)和非 NAFLD 患者发生 CVD 事件风险的观察性研究。主要终点是 CVD 死亡和(或)非致命性 CVD 事件。
NAFLD在不同年龄段的发生率
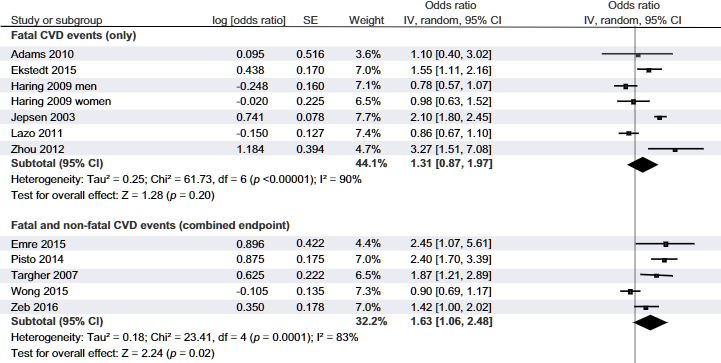
研究人员共确定了 36 项纵向研究,其汇总数据涵盖了 5,802,226 位中年人(平均 53 岁 [SD 7])和 99,668 例致命和非致命性 CVD 事件,中位随访时间为 6.5 年(IQR 5.0–10.2)。NAFLD 与致命或非致命 CVD 事件风险中等升高相关(汇总随机效应 HR 1.45,95% CI 1.31–1.61;I2=86.18%)。CVD 事件风险随着 NAFLD 的严重程度的增加而明显增加,尤其是纤维化阶段(汇总随机效应 HR 2.50,95% CI 1.68–3.71;I2=73.84%)。所有风险均独立于年龄、性别、肥胖指标、糖尿病和其他常见的心脏代谢风险因素。敏感性分析的结果与上述一致。
与NAFLD相关的致命或非致命性CVD事件风险
综上,NAFLD 与致命或非致命性 CVD 事件的长期风险增加有关。肝脏疾病越晚期,心血管疾病风险越高,尤其是纤维化阶段。该研究提供证据表明,NAFLD 可能是 CVD 发病和死亡的独立危险因素。
原始出处:
Mantovani Alessandro,Csermely Alessandro,Petracca Graziana et al. Non-alcoholic fatty liver disease and risk of fatal and non-fatal cardiovascular events: an updated systematic review and meta-analysis.[J] .Lancet Gastroenterol Hepatol, 2021, https://doi.org/10.1016/S2468-1253(21)00308-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#酒精性脂肪肝#
37
#GAS#
25
#非酒精性#
31
#AST#
28
#血管事件#
33
#Lancet#
24
#酒精性#
23
#Gastroenterol#
25
#心血管#NAFLD 与致命或非致命性 CVD 事件的长期风险增加有关。肝脏疾病越晚期,心血管疾病风险越高,尤其是纤维化阶段。该研究提供证据表明,NAFLD 可能是 CVD 发病和死亡的独立危险因素。
89
#心血管事件风险#
37