Eur Urol Oncol:高危上尿路尿道癌根治术后的肿瘤学监测
2022-05-23 AlexYang MedSci原创
作者建议在RNU后的第4年之前加强影像学检查的频率,即每半年一次,从第4年开始可以每年进行膀胱镜检查。
目前,根治性肾切除术(RNU)治疗上尿路上皮癌(UTUC)后适当的监测方案仍未得到很好的阐释。近日,来自意大利圣拉斐尔生命健康大学等单位的研究人员根据过往的膀胱癌(BCa)病史,评估了RNU后肿瘤监测的适当强度和时间。
研究人员根据欧洲泌尿外科协会(EAU)指南,从一个涉及八个欧洲转诊中心的前瞻性数据库中确定了1378名高危UTUC患者。根据EAU指南,监测方案是基于膀胱镜检查和横断面成像。
首先,研究人员根据目前EAU指南的建议,针对随访时间点评估了膀胱和其他部位复发(包括远处转移和局部区域复发)的非累积风险。然后,为了确定其他原因死亡(OCM)的风险超过复发的风险并可能停止随访的时间点,他们使用调整后的Weibull回归。
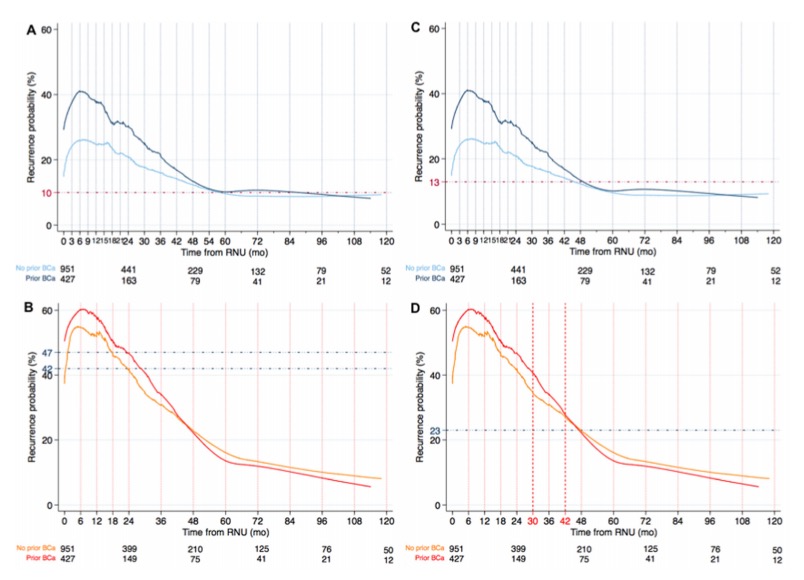
图1 在接受根治性肾输尿管切除术的高风险上尿路上皮癌患者中,(A和C)非累积性膀胱复发风险和(B和D)其他部位复发(切除术床,区域淋巴结和远处转移),根据既往膀胱癌史分层。
结果显示,随访的中位数为4年,分别纳入了427名和951名有和没有BCa病史的患者。在5年后,即在此之后每半年进行一次膀胱镜检查的时间点,膀胱复发风险为10%;在4年后,膀胱复发风险为13%。在2年后,也就是在此之后每半年进行一次影像检查的时间点,非既往BCa的非膀胱复发风险为42%,既往BCa的为47%;4年后,非膀胱复发风险为23%。在没有BCa病史的患者中,60岁以下的人应该在RNU后的10年内继续进行膀胱镜检查和影像学检查,70-79岁的患者应该在10年内只进行影像学检查,而80岁以上的患者由于OCM风险增加,可以停止肿瘤监测。该研究的局限性包括患者接受治疗和监测的时间相对较长。
综上所述,作者建议在RNU后的第4年之前加强影像学检查的频率,即每半年一次,在这个时间点之后,复发的风险几乎减半。鉴于RNU后4年和5年的复发风险相似,从第4年开始可以每年进行膀胱镜检查。在一些病例中,如果没有既往的BCa病史,可以停止肿瘤学监测。
原始出处:
Martini A, Lonati C, Nocera L, et al. Oncologic Surveillance After Radical Nephroureterectomy for High-risk Upper Tract Urothelial Carcinoma. Eur Urol Oncol. 2022 Apr 30
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#尿道#
46
#Oncol#
37
#尿道癌#
44
#肿瘤学#
27
#根治术#
38
#根治#
31