ASCO-2021速递: 哈佛大学:乳腺癌药物,可延长胶质母细胞瘤的无进展生存期
2021-06-07 Freeman MedSci原创
ASCO-2021速递: 哈佛大学:乳腺癌药物,可延长胶质母细胞瘤的无进展生存期
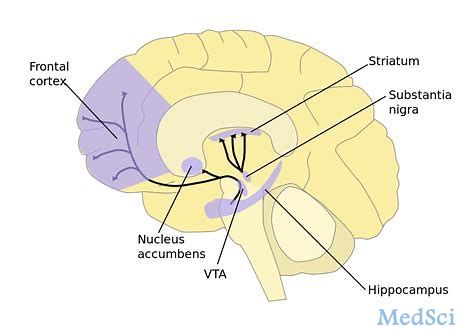
在大多数胶质母细胞瘤中,细胞周期蛋白D-CDK4/6-Rb途径被激活。Abemaciclib是一种有效的CDK4/6抑制剂,具有良好的脑部渗透性,被批准用于治疗HR+/HER2-乳腺癌。
为了有效评估Abemaciclib对新诊断的胶质母细胞瘤总生存期(OS)的潜在影响,并同时开发有关潜在的基因组生物标志物关联的信息,Abemaciclib被列为创新胶质母细胞瘤疗法个体化筛选试验(INSIGhT)的一个试验组。
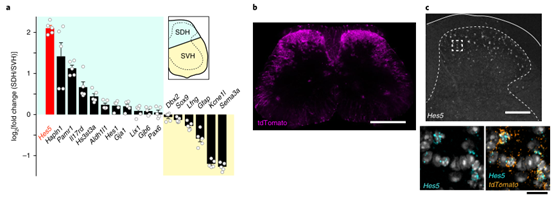
哈佛大学Dana-Farber癌症研究所Ligon, Brian Michael Alexander等人,设计的INSIGhT(NCT02977780)是一项II期平台试验,使用反应适应性随机化和深度基因组分析(response adaptive randomization and deep genomic profiling),以更有效地测试MGMT非甲基化胶质母细胞瘤的实验性药物,并有可能加速确定III期测试的新型疗法。
最初的随机化在abemaciclib、对照组和其他两个实验组之间是平等的,但随后的随机化是根据无进展生存期(PFS)确定的疗效进行调整。无效的试验组(Ineffective arms )被终止,而新的试验组则通过修改方案(attendment)加入。我们报告了已经完成招募的abemaciclib组的初步结果。
新诊断的MGMT非甲基化胶质母细胞瘤患者被随机分配,接受标准剂量的放化疗和辅助的替莫唑胺治疗,或标准放化疗后接受辅助的abemaciclib治疗(150-200mg,口服,BID)。
治疗持续到病情进展或出现不可接受的毒性。主要终点是OS,通过Kaplan Meier方法估计的对数rank检验来评估,I型误差为5%。 通过Cox模型计算HR。并探究了Abemaciclib疗效与细胞周期蛋白D-CDK4/6-Rb通路基因组改变之间的关系。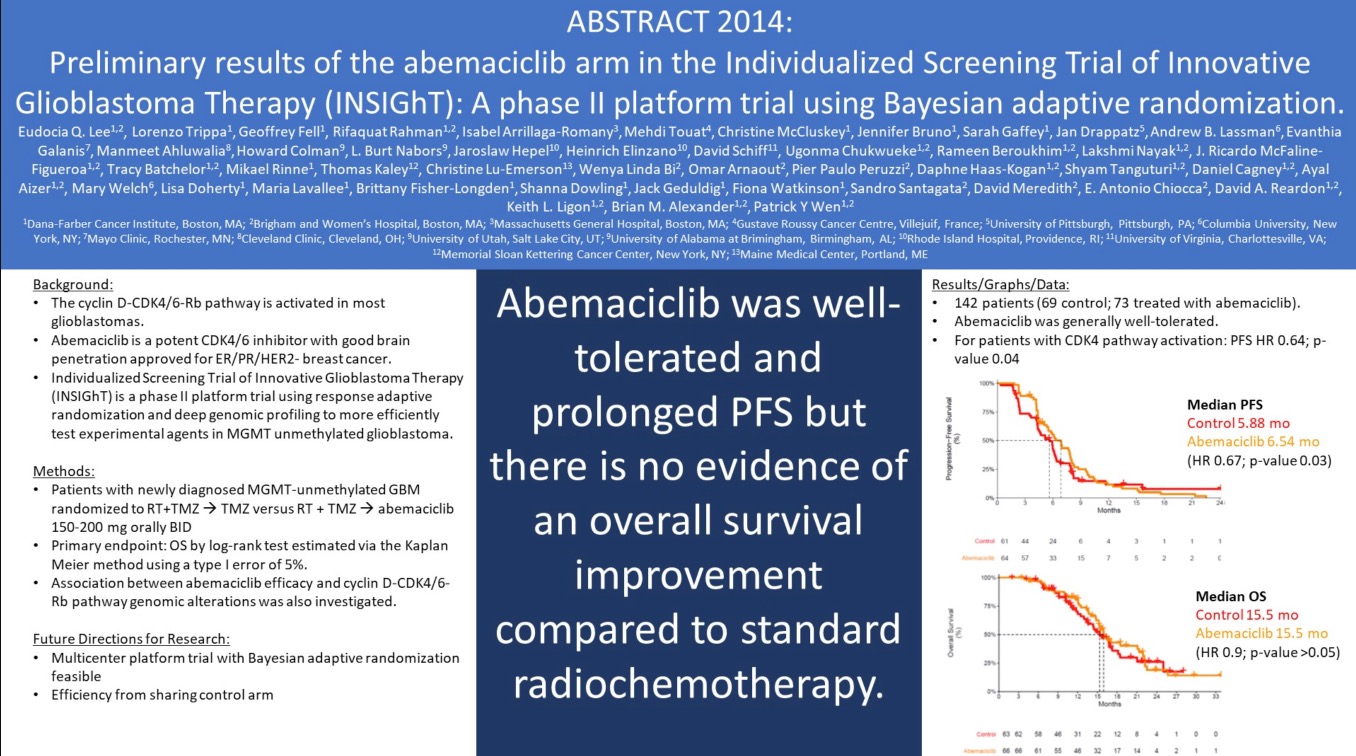
他们发现:共有142名患者(69名对照组;73名使用Abemaciclib治疗)。
Abemaciclib普遍耐受性良好,没有发现新的毒性信号。
与对照组(中位数5.88个月)相比,使用Abemaciclib的PFS明显更长(HR 0.67;p = 0.03,logrank检验)。对于CDK4途径激活的患者,PFS HR为0.64(P值=0.04)。
然而,与对照组(中位数15.5)相比,abemaciclib(中位数15.5)的总生存期没有明显改善(HR 0.9;p值>0.05)。
这个RCT的核心结论:Abemaciclib耐受性良好,延长了PFS,但没有证据表明与标准放化疗相比,总生存期有所改善。
原始出处;
Eudocia Quant Lee, Lorenzo Trippa, et al. Dana-Farber/Brigham and Women's Cancer Center, Harvard Medical School, Boston, MA; Brigham and Women's Hospital, Boston, MA; Dana-Farber Cancer Institute and Harvard Medical School, Boston, MA; Dana-Farber Cancer Institute/Brigham and Women's Hospital, Boston, MA
J Clin Oncol 39, 2021 (suppl 15; abstr 2014)
10.1200/JCO.2021.39.15\_suppl.2014
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#ASC#
50
#胶质母细胞#
46
#母细胞瘤#
36
#生存期#
46
#无进展生存期#
0
#细胞瘤#
37
#哈佛#
48