Microbiology Spectrum:“强大助攻”益生菌!可增强哮喘常规用药治疗效果!
2021-10-18 MedSci原创 MedSci原创
Microbiology Spectrum:补充益生菌能通过调节肠道微生物组和血清代谢组减轻哮喘症状
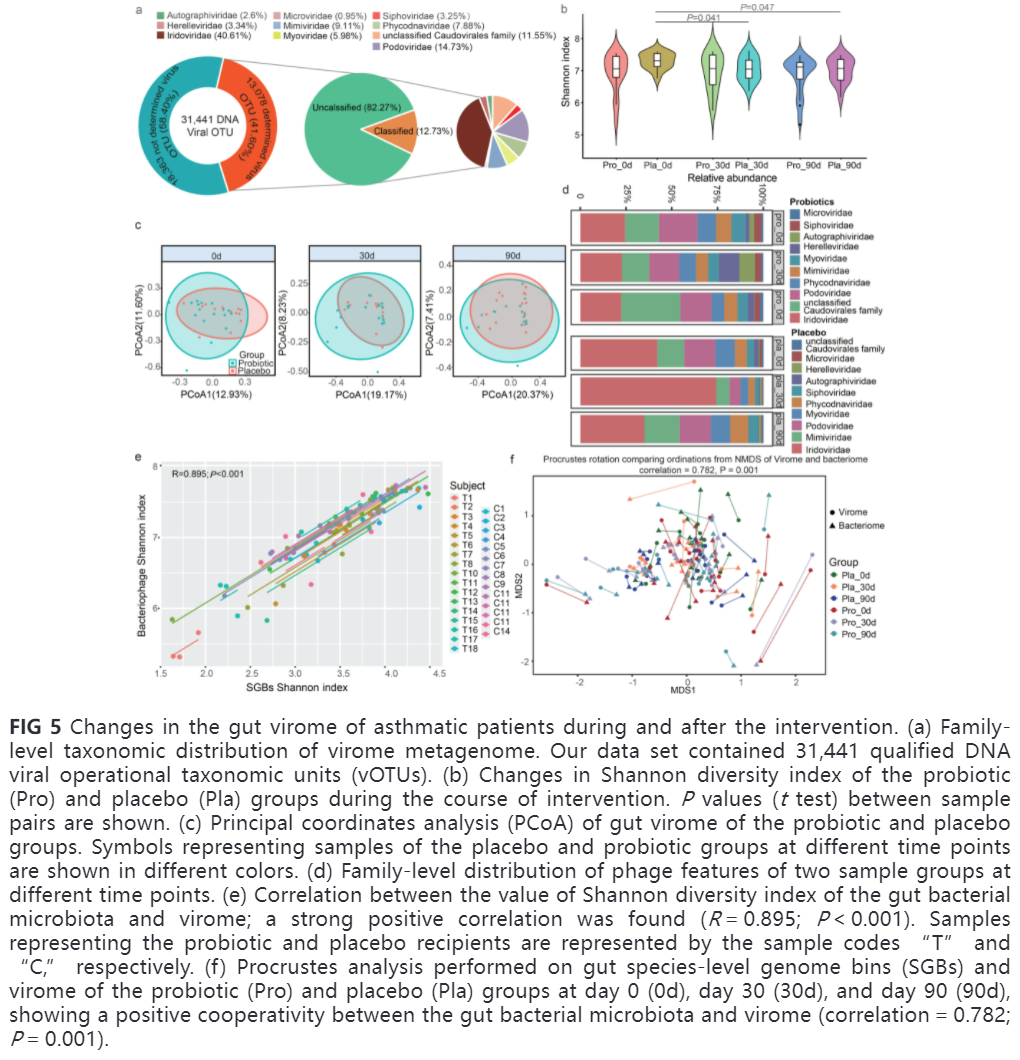
本研究旨在通过分析患者的临床指标、肠道菌群和血清代谢组的变化,评价m8益生菌缓解哮喘的临床疗效,并揭示其缓解哮喘症状的机制,为哮喘的发病机制和治疗、新型疾病管理策略的机制以及益生菌治疗的应用提供新的见解。
1、益生菌可改善哮喘相关症状。
为了评估益生菌治疗哮喘症状的辅助疗效,在第0、30和90天监测了多个临床参数,包括哮喘对照试验评分(ACT)、CaNO、呼气峰流量(PEF)、PEV1和FeNO,在第0天,益生菌组和安慰剂组在这些指标上没有观察到显著差异。
有趣的是,与安慰剂组相比,Probio-M8联合布地奈德/福莫特罗吸入剂在干预第30天显著降低FeNO水平(P = 0.049),并在干预结束时改善ACT评分(P = 0.023)。更重要的是,Probio-M8组在干预第30天显著降低了CaNO水平(P = 0.038),干预90天后这种效果更加明显(P = 0.001)。
此外,与第0天相比,干预前后Probio-M8组ACT评分显著升高,CaNO和FeNO水平降低(P < 0.05)。Probio-M8组与安慰剂组在肺功能指标(PEF、PEV1、PVC)和外周血嗜酸性粒细胞计数方面均未观察到辅助疗效(表S3)。m8益生菌组与安慰剂组各时间点血清IgE水平无显著差异;而安慰剂组的IgE水平在研究期间和研究结束时显著升高(P <0.003;图1 a)。提示m8益生菌辅助治疗可明显改善部分哮喘相关临床症状。
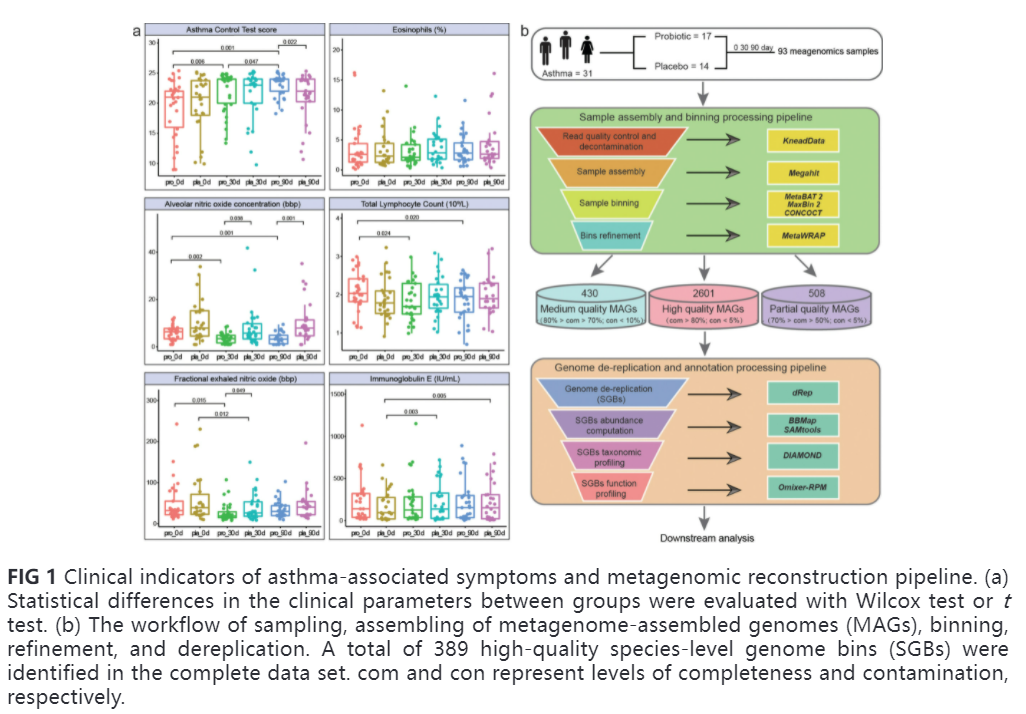
2、基因组的特性
在第0、30和90天,对31名受试者共93个样本进行了深入的MAGs分析。结果表明大多数基因组属于已知的微生物群落(图1b)。跟踪样品中的Probio-M8发现在益生菌组中,Probio-M8菌株的丰度逐渐增加,而在安慰剂组中则没有,这表明摄入的Probio-M8菌株可以很容易地通过消化道(图S2c)。
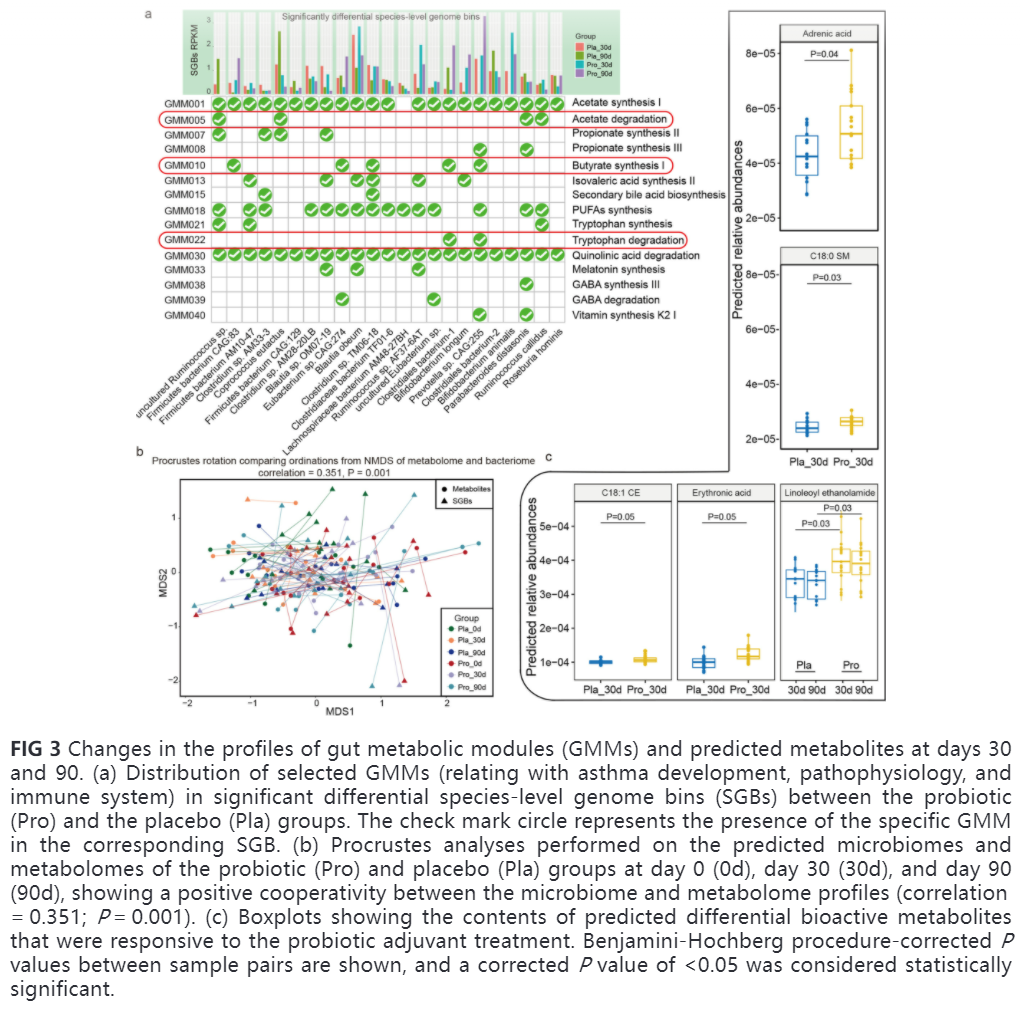
3、益生菌调节肠道菌群组成
Probio-M8组和安慰剂组在各时间点的α多样性和β多样性均无显著差异(P> 0.05,图2a和b)。然而,与第0天相比,安慰剂组的α多样性在第30和90天显著降低(P值分别为0.05和0.005),而Probio-M8组在整个试验期间保持稳定(图2a)。这表明摄入益生菌可能有助于维持肠道菌群多样性的稳定。此外,按年龄进行亚组比较时,各时间点的肠道菌群α / β多样性均无显著差异(成人:28 ~ 59岁;老年人:61岁至71岁;P >0.05;图S2d和e)。



本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#治疗效果#
52
#Bio#
41
#Biol#
47
#Micro#
44
#CRO#
47
#PE#
37