Blood:Flotetuzumab作为难治性AML患者的补救免疫疗法的疗效和安全性
2021-02-14 MedSci原创 MedSci原创
急性髓系白血病(AML)是一种高异质性疾病。虽然现已有多种获批治疗药物,但治愈率仍差强人意。大约50%的急性髓系白血病(AML)患者对诱导治疗无反应(原发诱导失败[PIF])或在6个月内复发(早期复发
急性髓系白血病(AML)是一种高异质性疾病。虽然现已有多种获批治疗药物,但治愈率仍差强人意。大约50%的急性髓系白血病(AML)患者对诱导治疗无反应(原发诱导失败[PIF])或在6个月内复发(早期复发[ER])。
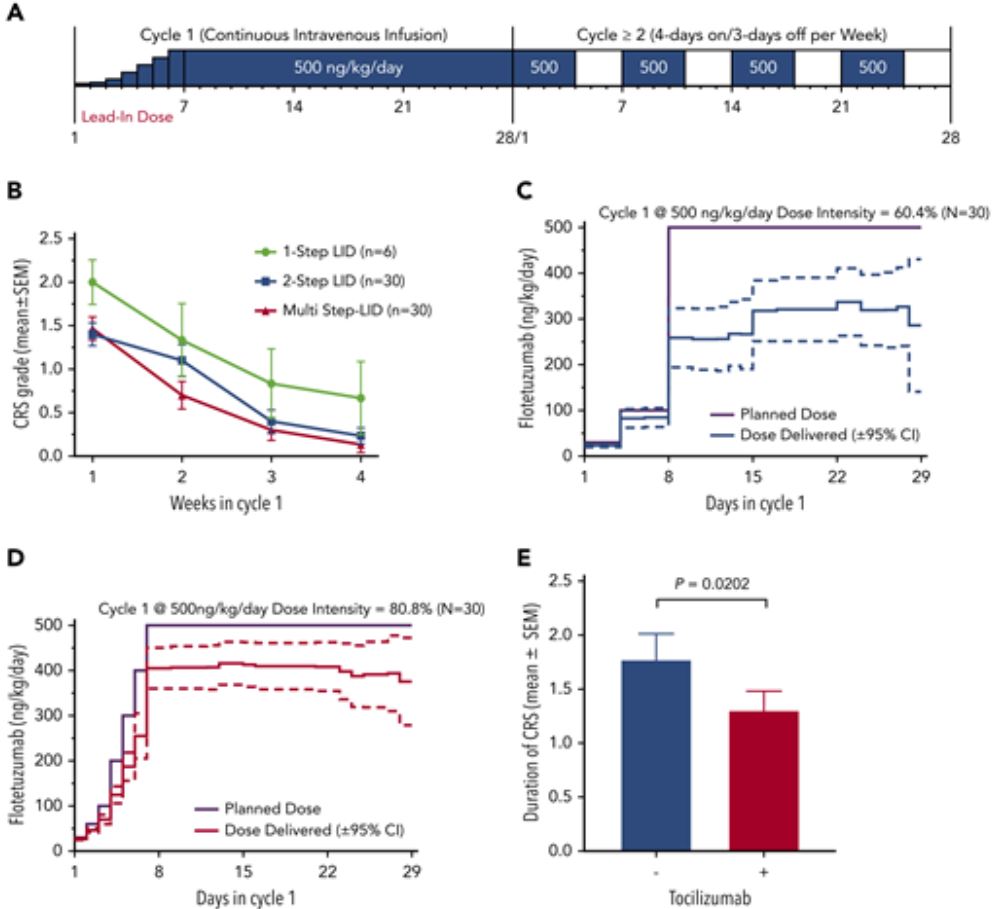
这是一项多中心、开放标签、1/2期研究,招募了88例成人复发性/难治性AML患者:42例在剂量探索队列,46例在推荐的2期剂量(RP2D)队列(500 ng/kg·日)。
研究人员发现,免疫浸润性肿瘤微环境与以阿糖胞苷为基础的化疗耐药和对氟替珠单抗(flotetuzumab,一种靶向CD3ε和CD123的双特异性DART抗体)的反应性相关。
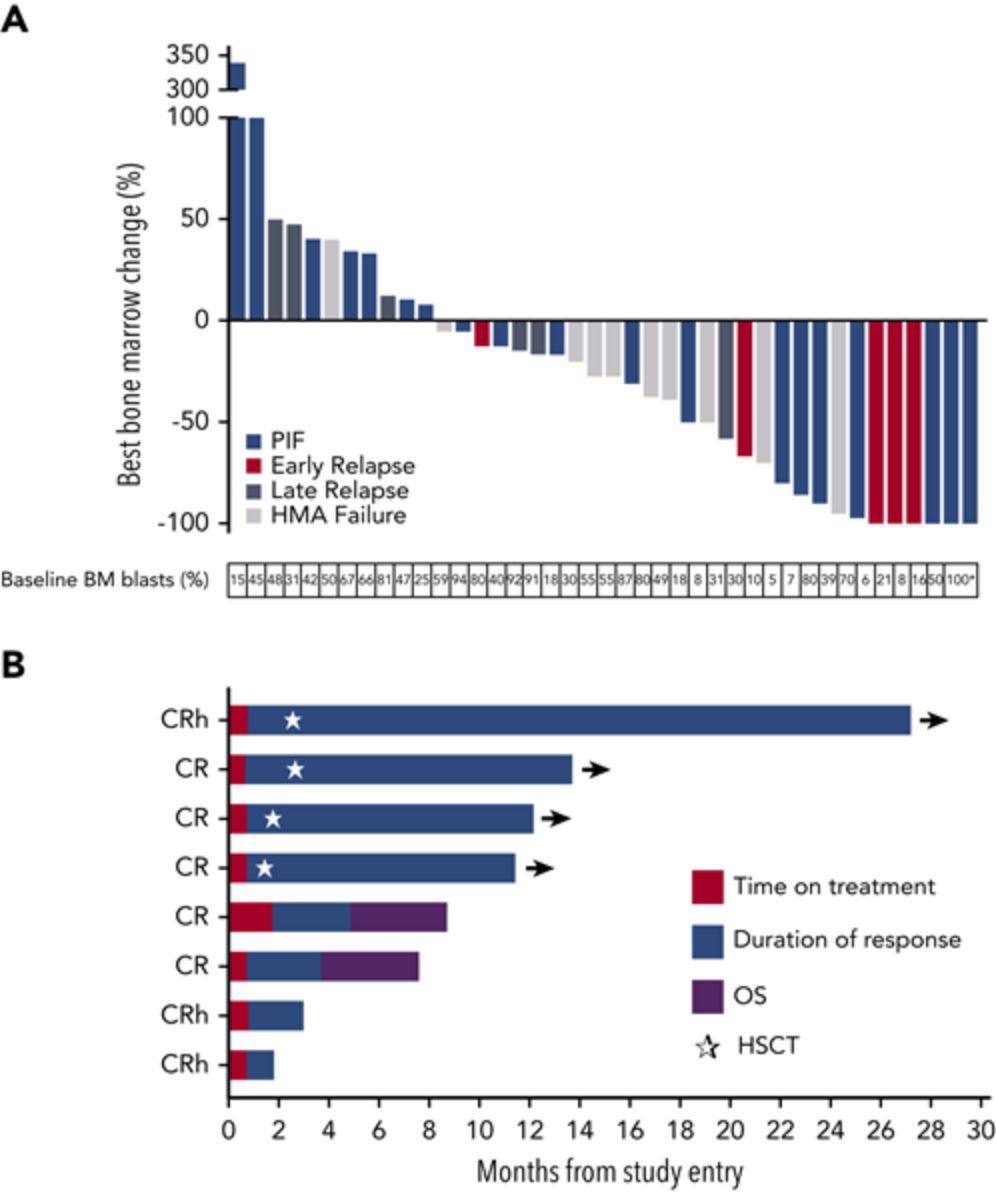
出现免疫浸润性TME的PIF/ER患者获得了临床治疗益处。在采用RP2D方案治疗的30例PIF/ER患者中,完全缓解(CR)和CR伴部分血液学恢复(CRh)率为 26.7%,总有效率(CR/CRh/CR伴血液学不完全恢复)为 30.0%。中位总生存期为 10.2个月(1.87~27.27),6个月和12个月生存率分别为75%(95%CI 0.450~1.05)和50%(0.154~0.846)。
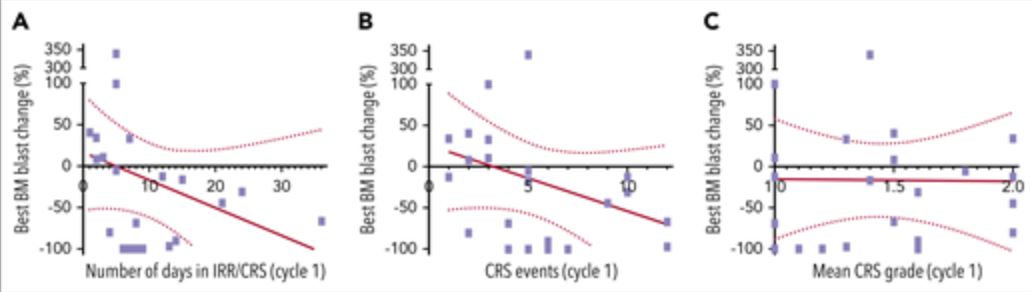
最常见的不良事件是输液相关反应(IRR)和细胞因子释放综合征(CRS),主要是1-2级。在第1周内分步给药、地塞米松预处理、迅速使用托珠单抗和临时剂量减少/中断可成功预防重度IRR/CRS的发生。
骨髓转录分析显示,简单的10基因签名即可以预测PIF/ER患者接受氟替珠单抗治疗的CRs(AUC=0.904),精准度明显优于ELN风险分类。
总之,氟替珠单抗(floteuzumab)代表了一种创新性的实验性治疗方法,在PIF/ER患者中展现出了可接受的安全性和令人鼓舞的治疗活性。
原始出处:
Uy Geoffrey L,Aldoss Ibrahim,Foster Matthew C et al. Flotetuzumab as salvage immunotherapy for refractory acute myeloid leukemia. Blood, 2021, 137: 751-762.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
34
#疗效和安全性#
35
#FLOT#
50
#难治性#
43
#TET#
31
涨知识
77
谢谢梅斯提供这么好的信息,学到很多
43