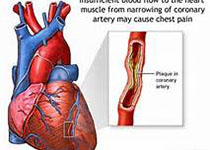
NEJM:急性冠状动脉综合征或PCI术后房颤患者的抗栓治疗
2019-04-18 xing.T 网络
由此可见,在近期急性冠状动脉综合征或PCI并服用P2Y12抑制剂治疗的房颤患者中,包含阿哌沙班(不含阿司匹林)的抗血栓治疗方案使患者出血少,住院次数少,缺血事件发生率与服用维生素K拮抗剂、阿司匹林或两者同时服用的个体没有明显差异。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#冠状动脉综合征#
51
#术后房颤#
38
#PCI术#
49
#综合征#
31
#PCI术后#
41
#房颤患者#
37
学习
101
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
45
学习谢谢分享
87