ASCO 2021:摘要概览与展望13|非小细胞肺癌专题研究速递(01)
2021-05-28 Oranhgy MedSci原创
ASCO 2021:摘要概览与展望12 | 阿斯利康最新数据支持通过更早治疗和改变患者体验来彻底改变癌症结局的雄心壮志
ASCO 2021:摘要概览与展望12 | 阿斯利康最新数据支持通过更早治疗和改变患者体验来彻底改变癌症结局的雄心壮志

研究1:多靶点细胞毒性T淋巴细胞(MCTL)联合特瑞普利单抗作为晚期非小细胞肺癌(NSCLC)二线治疗的单臂Ib期研究
背景
抗PD-1/PD-L1 mAb治疗已经在美国和欧洲被批准作为晚期NSCLC的二线治疗,因为与多西他赛相比有良好的耐受性和疗效。然而,客观反应率仅为20%左右。多靶点细胞毒T淋巴细胞(MCTL)可以恢复抗肿瘤免疫力,改善患者的治疗效果。将MCTL细胞与抗PD-1 mAb相结合,作为晚期NSCLC患者的二线治疗,可能会加强效果。
方法
研究人员开展单中心、开放标签、1b期的试验,即联合MCTL细胞和特瑞普利单抗(抗PD-1 mAb)作为晚期NSCLC的二线治疗。系统治疗患者每3周接受一次特瑞普利单抗,共12个周期,每3周接受一次MCTL细胞,共9个周期,然后接受特瑞普利单抗和MCTL细胞的维持治疗,直到疾病进展或出现不可接受的毒性。
结果
从2019年6月到2020年10月,14名年龄在43-70岁(中位年龄59岁)的患者入组。鳞癌/非鳞癌的比例为50%/50%。8人(57.1%)为男性,13人(92.8%)为ECOG PS=0-1,5人(35.7%)有胸腔积液,3人(21.4%)有骨转移。在13名可评估的患者中,客观缓解率(ORR)和疾病控制率(DCR)分别为38.4%和71.4%,在数据截止时,中位缓解持续时间(DOR)未达到(范围8.25m-NA),中位无进展生存期(PFS)为399天(范围192d-NA),中位总体生存期(OS)未成熟。不良事件(AEs)发生在5例(38.4%),没有发生≥3级的AEs事件。与免疫有关的AE是甲状腺功能低下(3,23%)和虚弱(2,15.4%)。目前正在分析与疗效和AEs相关的生物标志物。
结论
多靶点细胞毒性T淋巴细胞(MCTL)联合特瑞普利单抗作为晚期NSCLC的二线治疗,因为耐受性好,疗效令人鼓舞。需要进一步的研究来证实这些结果。
详情参见:多靶点细胞毒性T淋巴细胞(MCTL)联合特瑞普利单抗作为晚期非小细胞肺癌(NSCLC)二线治疗的单臂Ib期研究
研究2 :晚期非小细胞肺癌(NSCLC)和头颈部鳞状细胞癌(HNSCC)的放疗(RT)引爆免疫疗法。II期临床试验的中期分析
背景
临床前模型证明,联合RT和免疫检查点抑制剂(ICI)会产生与肿瘤反应性群体相关的特定CD8+T细胞表型,从而产生明显的肿瘤反应。顺序治疗可以使放射线从免疫无法进入的区域释放肿瘤抗原,并通过ICI提供强大的抗肿瘤免疫反应。该研究报告了评估该组合的疗效和安全性的II期临床试验的中期分析。
方法
已开始使用FDA批准的单药ICI的晚期NSCLC和HNSCC患者符合条件。患者在第一次ICI用药后14天内接受SBRT(BED>100Gy)或30Gy分次RT,以3维剂量送入单一转移部位。主要目标是6个月的PFS,次要目标是安全性和耐受性、1年PFS和OS。这项中期分析是在43名患者入组后进行的。
结果
在2017年10月至2021年1月期间,有43名患者入组,38名患者被纳入本分析。中位年龄为62岁;26名患者为男性。9名患者接受ICI治疗NSCLC一线,7名NSCLC二线,22名HNSCC二线。24名患者接受了pembrolizumab,14名接受了nivolumab;21名接受了SBRT,17名接受了分次RT。
无进展性疾病(PD)的患者的中位随访时间为11.8月(范围:2.7 - 31.4月)。10名患者退出研究,7名继续治疗。15人死亡,26人有PD。14名患者死于恶性肿瘤,1名患者的死因不明。6个月PFS为49.19%,中位PFS为5.5个月。
21名受试者中报告了52例3-5级不良事件(AEs)。最常见的是转氨酶(n=15)、淋巴细胞减少症(n=8)和消化道副作用(n=4)。与治疗有关的AEs包括19个3级事件,没有一个是4/5级的。两个5级AE来自PD(口腔出血和未指明)。有20个1/2级和3个3级的免疫相关不良事件(IRAEs)。没有4/5级IRAEs的报告。两名患者因3级转氨酶而停止治疗。
结论
中期分析显示,6个月的PFS是可以接受的,大多数患者是二线转移性HNSCC,在Checkmate-141/KEYNOTE-040试验中,其mPFS为2.1-2.3个月,mOS为7.7-8.4个月。因此,该组合具有进一步的意义,应征者将继续达到目标。联合治疗是可以容忍的,没有意外的AE。大部分的死亡是由于疾病的进展。没有治疗相关的4/5级不良事件的报告。两名患者因3级IRAE而停止治疗。
详情参见:晚期非小细胞肺癌(NSCLC)和头颈部鳞状细胞癌(HNSCC)的放疗(RT)引爆免疫疗法。II期临床试验的中期分析
研究3:晚期非小细胞肺癌(NSCLC)患者自体细胞因子诱导的杀伤性(CIK)细胞免疫疗法联合辛硫磷加化疗的单臂Ib期研究
背景
免疫检查点抑制剂加化疗对没有靶向突变的晚期非小细胞肺癌(NSCLC)患者有效。自体细胞因子诱导的杀伤细胞(CIK)可以恢复抗肿瘤免疫力,从而改善患者的治疗效果。将CIK细胞与抗PD-1 mAb加化疗相结合可能会加强晚期NSCLC患者的治疗效果。
方法
这是一项针对 IIIB-IV 期 NSCLC 患者的 CIK 细胞联合sintilimab(抗 PD-1 mAb)加化疗的单中心、开放标签、1b 期试验。全身治疗初治患者每 3 周接受一次含铂双药化疗、sintilimab和CIK细胞加化疗。持续4个周期,然后sintilimab和CIK细胞的进行维持治疗,直到疾病进展或出现不可接受的毒性。
结果
从2019年5月到2021年1月,34名患者(19名鳞癌,15名非鳞癌NCSLC)入选,年龄46~73岁(中位年龄64岁)。
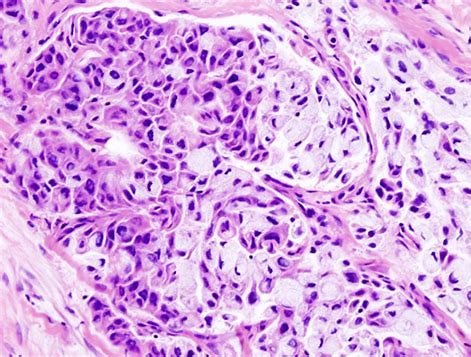
在32名可评估的患者中,ORR为81.3%(鳞状细胞癌为73.7%,非鳞状NSCLC为92.3%),DCR为100%。在通过RECIST评估的25例PR中,有5例(23.1%)通过PET-CT证明有CMR。在3名有脑转移的患者中,2名患者颅内CR,1名为PR。中位随访7.5个月,中位DOR未达到(范围0.5m-NA),中位PFS和OS未成熟。3级或以上TRAE包括肺炎(n = 3);血小板减少,白细胞减少(n = 2各);贫血,吞咽困难,心肌病,皮疹(n = 1)。正在分析的与疗效和AEs相关的生物标志物和亚组包括TMB、PDL1表达、TILs的分布、细胞因子等。
结论
CIK细胞治疗联合Sintilimab和化疗的耐受性良好,显示出令人鼓舞的疗效。需要进一步研究以证实这些初步结果。
详情参考:晚期非小细胞肺癌(NSCLC)患者自体细胞因子诱导的杀伤性(CIK)细胞免疫疗法联合辛硫磷加化疗的单臂Ib期研究
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#ASC#
37
#专题#
37
#非小细胞#
31
好文章
63
好文章
56
好文章,学习了
59