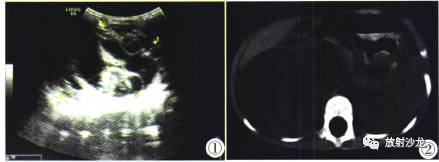
小儿特发性肺动脉高压1例
2017-12-20 熊长明 肺血管病
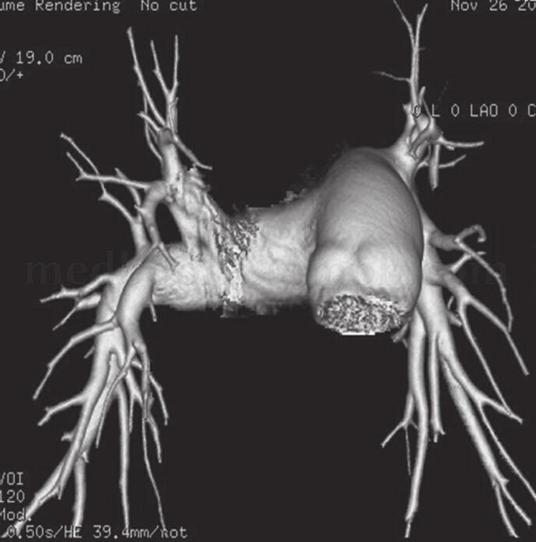
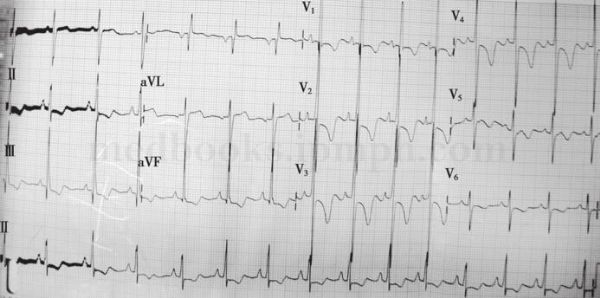
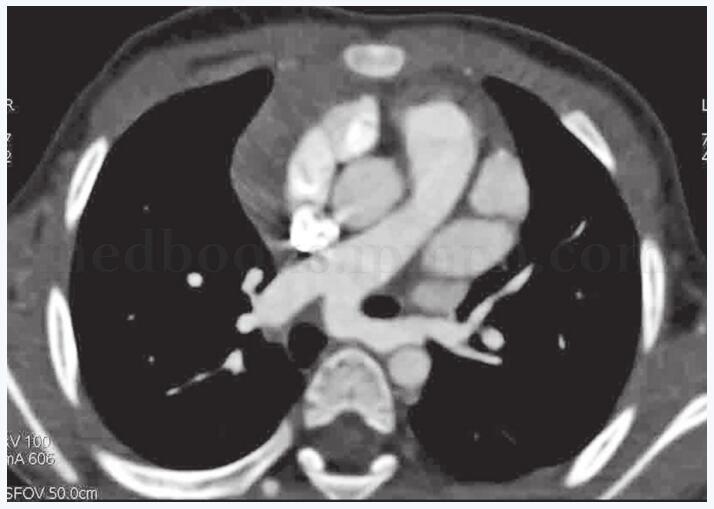
患儿,女,9岁。因活动后心悸、气短入院。其父亲死于肺动脉高压,家属中无其他人有类似疾病。查体:无发绀,左胸稍隆起,心界不大,心尖搏动呈抬举性,双肺未闻及干湿啰音。患儿发病的原因是否与遗传性的因素有关呢?

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#动脉高压#
0
#特发性#
37
#特发性肺动脉高压#
46
学习了受益匪浅
76
肺动脉高压表面是罕见病,事实上临床上并不少见,治疗药物虽然有一些,但是整体仍然不理解,可能未来需要采用综合治疗措施。
40
学习
78
学习了新知识
74