Lancet Oncol:CD40激动性单克隆抗体APX005M联合化疗治疗转移性胰腺癌
2021-01-06 Nebula MedSci原创
对于转移性胰腺腺癌,标准化疗的表现仍差强人意。
对于转移性胰腺腺癌,标准化疗的表现仍差强人意。激动性CD40单克隆抗体联合化疗科诱导小鼠体内T细胞依赖性的肿瘤消退,提高生存率。该研究旨在评估APX005M(sotigalimab)和吉西他滨联合nab-紫杉醇和或无纳武单抗治疗胰腺癌患者的安全性,以确定推荐的2期剂量。
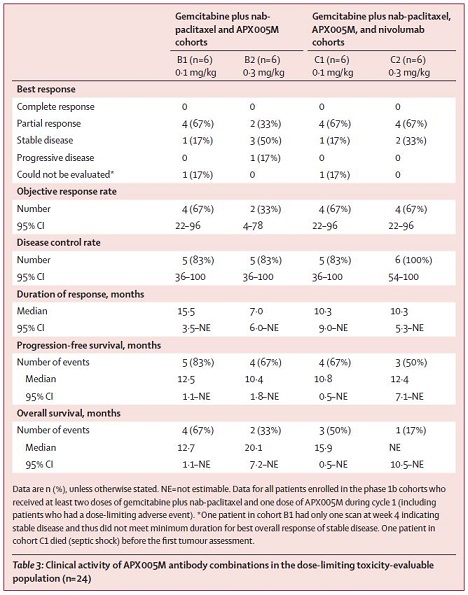
该研究是一项非随机、开放标签、多中心、多组的1b期试验,招募年满18岁的未治疗过的转移性胰腺癌患者。所有患者都接受吉西他滨(1000 mg/m2,静滴)和nab-紫杉醇(125 mg/m2,静滴)治疗。B1组和C1组的患者接受0.1 mg/kg的APX005M(静滴)治疗,B2组和C2组接受0.3 mg/kg的APX005M(静滴)治疗。C1组和C2组的患者还接受纳武单抗(240 mg)治疗。主要终点有不良反应发生率和剂量限制性毒性(DLT),并确定APX005M的2期推荐剂量。客观缓解率为次要终点。
2017年8月22日-2018年7月10日,筛选了42位患者,其中30位被纳入本研究,接受了至少一剂量的研究药物;24位为DLT可评估性,中位随访了17.8个月(B1组 22.0个月、B2组 18.2个月、C1组 17.9个月、C2组 15.9个月)。观察到两例DLT,均是发热性中性粒细胞减少症,分别发生在B2组(3级)和C1组(4级)的各一位患者。
最常见的3-4级治疗相关的不良反应事件有淋巴细胞计数减少(20例[67%];B1组、B2组、C1组、C2组分别有5例、7例、4例、4例)、贫血(11[37%];2例、4例、1例、2例)和中性粒细胞减少(9例[30%];3例、3例、1例、2例)。30位患者中有14位(47%;B1组、B2组、C1组各一例,C2组 2例)患者发生了治疗相关的严重不良反应。最常见的严重不良反应为发热(6例[20%];B2组 1例、C1组 3例、C2组 2例)。有两例化疗相关的死亡(死于不良反应:B1组1例败血症、C1组1例败血症休克)。
APX005M的推荐2期剂量为0.3 mg/kg。24例DLT可评估患者中有14位(58%)获得了缓解(B1组、C1组、C2组各一例,B组有2例)。
APX005M和吉西他滨联合nab-紫杉醇和或无纳武单抗治疗胰腺癌患者的耐受性良好,而且表现出了一定的临床活性。如果在后期临床试验中得到了验证,则该治疗方案或可替代单标准化疗方案用于这类患者人群。
原始出处:
Mark H O'Hara, et al. CD40 agonistic monoclonal antibody APX005M (sotigalimab) and chemotherapy, with or without nivolumab, for the treatment of metastatic pancreatic adenocarcinoma: an open-label, multicentre, phase 1b study. The Lancet Oncology. January 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Lancet#
32
#克隆#
38
#APX005M#
35
#CD4#
42
#Oncol#
0
#转移性#
25
#转移性胰腺癌#
38
#联合化疗#
38
顶刊就是不一样,质量很高,内容精彩!学到很多
52
谢谢梅斯分享这么多精彩信息
50