JAD:太极拳辅助治疗老年抑郁症对脑连接的影响
2022-08-01 影像小生 MedSci原创
在GD治疗中,非药理学辅助治疗,如TCC,可能会增强DMN连接改变,从而改善抑郁症状和心理弹性。
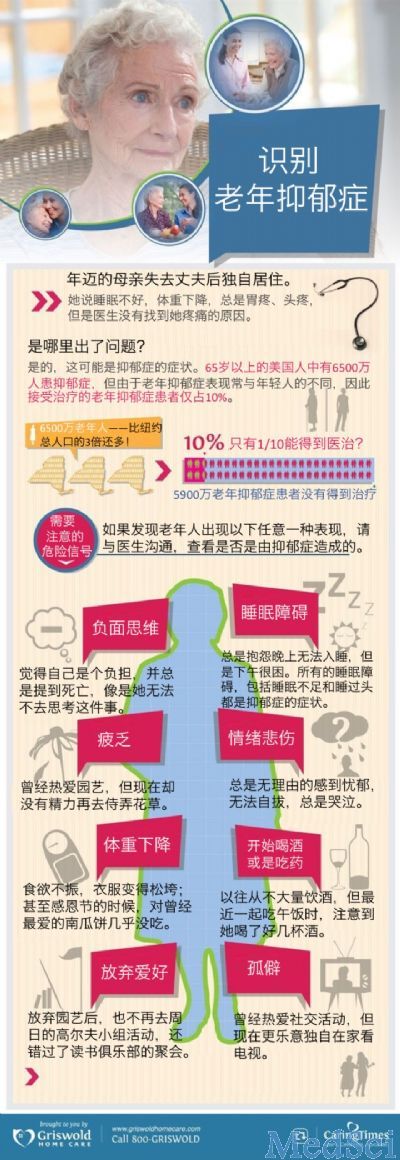
与年轻抑郁症患者相比,老年抑郁症(GD)与显著的医学共病、认知障碍和次优治疗反应相关。迫切需要更有效的治疗方法来改善GD的情绪、认知和生活质量。由于身心干预,如太极,可以减少负面情绪和全身炎症,并改善身心健康,并显示出对抑郁、焦虑和一般压力管理的有益效果,它们构成了一种很有希望的抗抑郁药物辅助治疗,以提高治疗效果。太极拳作为抗抑郁药物治疗的辅助手段,在改善老年抑郁症(GD)患者的总体健康状况方面优于健康教育和健康训练(HEW)。
Lisa A.Kilpatrick等在JAD发表研究文章,探讨TCC和HEW联合抗抑郁药物治疗GD患者的脑连接改变。
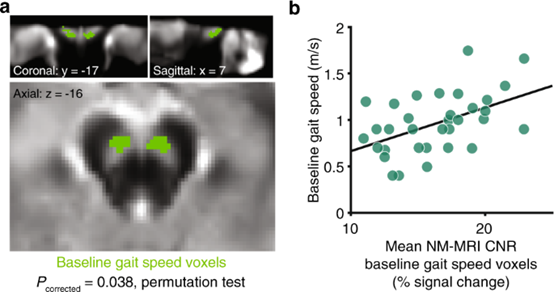
40例GD患者在稳定的抗抑郁药物治疗下进行了12周的TCC训练(n=21)或HEW训练(n= 19),并完成了基线和3个月的随访静息状态磁共振成像扫描。通过一般线性模型评估干预后包裹间连通性变化组内和组间差异。采用偏最小二乘相关分析评估显著连接变化与症状/弹性改善之间的关系。
结果如下:

与太极拳训练相比,与健康教育和健康训练的连通性增加更大(corrected_p < 0.05)
与HEW相比,TCC的连接显著增加(FDR校正p<0.05)观察到167对成对连接,最常见的涉及默认网络(DMN)。在两组中,主要涉及DMN区域的连接增加与症状/恢复能力的改善显著且正相关。
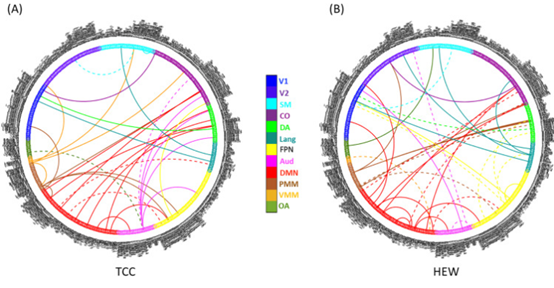
与症状改善和恢复能力相关的连接更改(bootstrap_p < 0.05)
该研究提供了初步证据,表明非药理学辅助药物,如TCC,可能在GD治疗中增强DMN连接变化,这与抑郁症状和心理弹性的改善有关。未来的研究应该在更多的患者中,通过更长的随访时间来研究这些神经改变在症状改善中的作用。
原文出处
Impact of Tai Chi as an adjunct treatment on brain connectivity in geriatric depression
https://www.sciencedirect.com/science/article/pii/S0165032722008175.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#老年抑郁症#
41
#太极#
60
#太极拳#
0
学习了,谢谢分享
50