Curr Eye Res:视网膜脱离和增殖性玻璃体视网膜病变中抗视网膜抗体的水平
2018-03-22 cuiguizhong MedSci原创
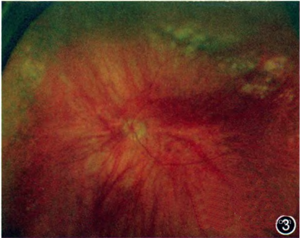
日本仙台东北大学医学研究院眼科的Ichinohasama R近日在Curr Eye Res发表了一项工作,他们研究了眼内抗视网膜抗体与孔源性视网膜脱离(RRD)和增殖性玻璃体视网膜病变(PVR)患者的临床测量之间的相关性。
日本仙台东北大学医学研究院眼科的Ichinohasama R近日在Curr Eye Res发表了一项工作,他们研究了眼内抗视网膜抗体与孔源性视网膜脱离(RRD)和增殖性玻璃体视网膜病变(PVR)患者的临床测量之间的相关性。
他们从RRD患者、PVR患者和黄斑裂孔对照者中收集房水和玻璃体样本。对总蛋白(TP)、IgG和抗视网膜抗体的水平分别用二辛可宁酸测定法、酶联免疫吸附测定法和斑点印迹测定等方法进行研究。使用Pearson's相关分析对这些测量参数之间的相关性进行评估。方差分析后使用事后检验或Student t检验来比较组间差异。

结果他们发现,抗视网膜抗体和IgG水平相互关联(P <0.010)。 PVR患者的IgG浓度在房水(P <0.001)和玻璃体(P <0.001)中均高于对照组,但在RRD患者中无此现象。相反,来自RRD和PVR患者的两种眼组织样本中的TP水平和抗视网膜抗体水平与对照组之间没有显着差异。在亚组分析中,玻璃体抗视网膜抗体水平与黄斑裂变RRD / PVR手术后重新附着的黄斑中的平均黄斑厚度相关(P = 0.012)。此外,术后囊样黄斑水肿患者的玻璃体抗视网膜抗体水平高于未患者(P = 0.009)。
因此,他们认为,在RRD或PVR手术干预后,眼内黄斑病变的玻璃体内抗视网膜抗体增加。
原文出处:
Ichinohasama, R., et al., Levels of Anti-Retinal Antibodies in Retinal Detachment and Proliferative Vitreoretinopathy. Curr Eye Res, 2018: p. 1-6.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#eye#
37
#玻璃体#
0
#视网膜病变#
35
#视网膜#
28
学习了很有用
0
谢谢分享.学习了
64
学习学习.继续关注
62
学习了新知识
56
学习了新知识
59
学习了新知识
25