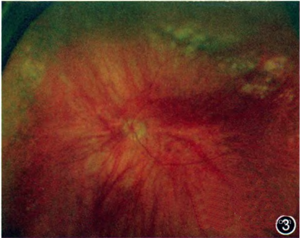
Ophthalmologica:视网膜脱离患者的玻璃体视网膜下液体中凝血酶的生成
2018-04-08 cuiguizhong MedSci原创
荷兰鹿特丹眼科医院的Mulder VC近日在Ophthalmologica发表了一篇文章,他们测量了孔源性视网膜脱离(RRD)患者的玻璃体和视网膜下部液体(SRF)中凝血酶原片段(F1 + 2)和凝血酶-抗凝血酶复合物(TAT)的活性,并进一步证实了他们较早之前发现的增生性玻璃体视网膜病变(PVR)患者中凝血酶活性上升。
荷兰鹿特丹眼科医院的Mulder VC近日在Ophthalmologica发表了一篇文章,他们测量了孔源性视网膜脱离(RRD)患者的玻璃体和视网膜下部液体(SRF)中凝血酶原片段(F1 + 2)和凝血酶-抗凝血酶复合物(TAT)的活性,并进一步证实了他们较早之前发现的增生性玻璃体视网膜病变(PVR)患者中凝血酶活性上升。

他们使用Enzygnost免疫分析法测量31个玻璃体和16个SRF样品中的F1 + 2和TAT活性。结果他们发现,所有RRD患者的玻璃体中,F1 + 2和TAT水平显着高于黄斑裂孔或黄斑皱褶的患者。然而,在可能发展为PVR的患者,或是PVR的患者,以及在两者都不是仅是简单的RRD的患者之间,玻璃体中F1 + 2(Kruskal-Wallis p = 0.963)和TAT(p = 0.516)都没有发现存在显着的差异。
因此,他们认为,对F1 + 2和TAT的分析证实了RRD患者的玻璃体和SRF中的凝血酶活性明显升高。TAT和α2-巨球蛋白之间不平衡的凝血酶调节机制可能解释了他们以前研究结果的差异。
原文出处:
Mulder, V.C., et al., Thrombin Generation in Vitreous and Subretinal Fluid of Patients with Retinal Detachment. Ophthalmologica, 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#视网膜#
32
#玻璃体#
0
#THA#
39
不错的文章值得拥有
78