PHILIPS每日一例:肝豆状核变性合并原发性肝癌1例
2022-09-01 放射沙龙 中国中西医结合影像学杂志
急、慢性肝炎或脂肪肝症状,最终可发展至肝硬化。因此,肝脏既是HLD的始发部位,又是最主要的受累器官。然而,HLD并发原发性肝癌却非常罕见,其机制至今未能完全阐明。
男,55 岁,因“反复腹胀伴双下肢肿胀7 年,加重半年”于2012 年7 月入院。查体:肝病面容,腹部膨隆,脾脏肋下可及,双下肢肿胀。患者2005 年因不明原因腹胀来我院就诊,无乙肝病史,肝功能检查示ALT 270 U/L,AST 185 U/L,血铜蓝蛋白0.08 g/L,铜氧化酶0.02 活力单位/L,24 h尿铜1 303.02 μg/L,角膜K‐F环阳性,腹部彩超示肝硬化、腹水。临床确诊为肝硬化、肝豆状核变性(hepatolenticular degeneration,HLD),予以排铜、保肝治疗,出院后病情反复,于2011 年7 月因脾功能亢进行脾脏部分栓塞术。近半年患者腹胀加重,2012 年7 月我院上腹部CT 示肝左叶占位性病变(肝癌可能)、腹膜多发转移性结节(见图1);AFP 5 880 ng/ml;HBsAg 阴性,HCV 阴性。患者拒绝活检,但其临床症状、CT表现及实验室检查符合原发性肝癌的临床诊断标准,故诊断为:① 原发性肝癌;② 肝硬化;③ HLD。

图1 CT平扫示肝左叶占位性病变、腹膜小结节
于2012 年8 月行TACE 治疗,术中见肝左动脉增粗、迂曲,其分支明显增多、紊乱,远端可见大量新生血管,实质期可见团块状肿瘤染色,局部可见动静脉瘘(见图2,3),予以吡柔比星(THP)20 mg+丝裂霉素(MMC)10 mg+超液态碘化油10 ml的混合乳剂灌注,碘油沉积佳,动静脉瘘消失。介入术后1 个月复查CT 示肝左叶病灶碘油沉积尚可,两侧肾上腺可见肿块(考虑为转移)(见图4~8)。现拟继续行介入治疗、定期随访。

图2,3 肝动脉造影示肝左动脉迂曲,远端可见大量新生血管,实质期可见团块状肿瘤染色
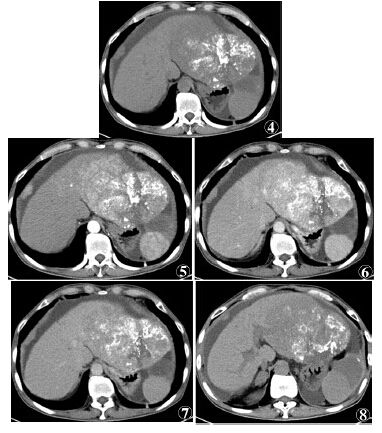
图4~7 肝动脉灌注化疗栓塞术后复查,肝脏CT平扫及3期增强扫描示肝左叶肿块碘油沉积尚可,增强扫描后动脉期明显不均匀强化;腹膜多发强化结节,;图8 CT平扫示右侧肾上腺转移瘤
讨论
HLD,又称Wilson病,是一种常染色体隐性遗传性铜代谢障碍性疾病,由于缺乏P型铜转运酶或功能下降,造成铜蓝蛋白合成障碍及铜离子转运减弱,铜异常沉积在肝、肾、脑、角膜等组织,引起一系列临床症状。HLD临床表现复杂,分以下5型:① 肝型;② 脑型或神经型;③ 肾型与骨骼型;④ 溶血型;⑤ 发热型。肝型症状轻重不一,大多表现为肝炎、肝硬化,重者可发生肝功能衰竭。
研究证实,HLD患者游离的铜离子在肝细胞浆大量蓄积并引起肝脏损害,随着肝铜的蓄积逐渐达到饱和,游离铜从肝细胞浆进入溶酶体内,引起肝细胞弥漫性肿胀、坏死和小叶中心静脉周围纤维组织增生,临床出现急、慢性肝炎或脂肪肝症状,最终可发展至肝硬化。因此,肝脏既是HLD的始发部位,又是最主要的受累器官。然而,HLD并发原发性肝癌却非常罕见,其机制至今未能完全阐明。
实验研究证明,给雄性大鼠静注或皮下注射铜或醋酸铜使肝铜水平升高,肝癌启动基因被抑制,胸腺嘧啶脱氧核苷合成DNA减少;现多数学者推测可能是肝铜沉积后,铜对肝癌的基因启动有“保护性”的抑制作用,因此HLD合并肝癌报道非常罕见。综上所述,尽管HLD合并原发性肝癌非常罕见,但是临床工作中仍应足够重视,对HLD患者定期随访,一旦发现异常病灶应尽早确诊、积极治疗,以改善预后。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#原发性#
64
#原发性肝癌#
63
#iPS#
58
#变性#
46