J Clin Oncol:Brentuximab Vedotin联合AVD一线治疗早期不良霍奇金淋巴瘤的疗效优于标准疗法
2022-08-03 MedSci原创 MedSci原创
与标准的ABVD方案相比,BV-AVD方案可显著改善早期不良霍奇金淋巴瘤患者的PET阴性率
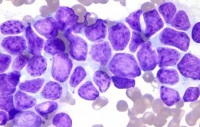
早期不良霍奇金淋巴瘤患者预后仍不理想。BREACH研究评估了Brentuximab vedotin联合多柔比星、长春新碱和达卡巴嗪 (BV-AVD) 在先前未治疗过的早期不利霍奇金淋巴瘤中的疗效和安全性。
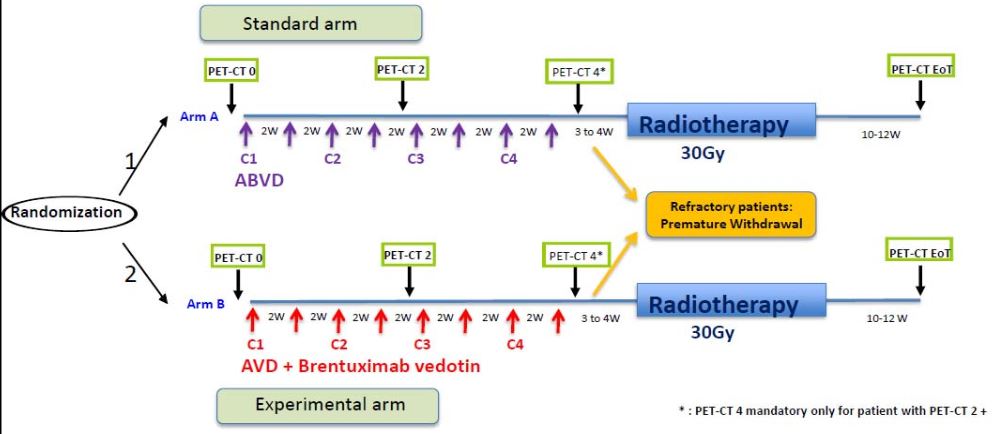
BREACH研究是一项多中心、随机、开放标签的II期试验,招募了18-60岁的有≥1个不良EORTC/LYSA标准因素的早期奇金淋巴瘤患者,随机(2:1)分成两组,分别接受4个疗程的BV-AVD治疗,或标准的多柔比星、博来霉素、长春新碱和达卡巴嗪(ABVD)治疗,继以30Gy放疗。主要终点是两个疗程后正电子发射断层扫描 (PET) 缓解率。该研究旨在测试两个疗程的BV-AVD后PET阴性率是否优于75%。
研究流程
2015年3月至2016年10月期间,共招募了170位患者。两个疗程后,该研究的主要终点得以实现:BV-AVD组的PET阴性率为82.3%(93/113),ABVD组的PET阴性率为75.4%(43/57)。BV-AVD组和ABVD组的2年无进展生存率分别是97.3%和92.6%。高总代谢肿瘤体积与显著缩短的PFS相关(HR 17.9,p<0.001)。BV-AVD组和ABVD组中高总代谢肿瘤体积患者的2年无进展生存率分别是90.9%和70.7%。
综上,与标准的ABVD方案相比,BV-AVD方案可显著改善早期不良霍奇金淋巴瘤患者的PET阴性率。
原始出处:
Luc-Matthieu Fornecker, et al. Brentuximab Vedotin Plus AVD for First-Line Treatment of Early-Stage Unfavorable Hodgkin Lymphoma (BREACH): A Multicenter, Open-Label, Randomized, Phase II Trial. Journal of Clinical Oncology. https://ascopubs.org/doi/figure/10.1200/JCO.21.01281
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
52
#标准疗法#
34
#Oncol#
35
#AVD#
51
#Brentuximab#
45
#vedotin#
38