JAMA:沙库巴曲缬沙坦钠对轻度心力衰竭患者实验室指标及运动能力的影响
2021-11-17 MedSci原创 MedSci原创
对于左室射血分数40%以上的心力衰竭患者,与标准的肾素-血管紧张素系统抑制剂治疗或安慰剂相比,沙库巴曲缬沙坦钠治疗可降低血浆N-末端脑钠肽前体水平,但对6分钟步行距离无显著改善作用

沙库巴曲缬沙坦钠是一种治疗心衰的药物,2015年7月获得了美国FDA批准上市,可降低成人慢性心衰患者心血管死亡和心衰住院风险。近日研究人员考察了沙库巴曲缬沙坦钠对轻度降低或左室射血分数保留(LVEF>40%)心衰患者部分替代终点标志物结果的影响。
本次研究考察沙库巴曲缬沙坦钠对轻度心衰患者NT-proBNP、6分钟步行距离、生活质量以及其他药物指标的影响,为期24周,为双盲平行对照研究,在32个国家396个中心开展,包含2572名心力衰竭患者,患者的LVEF在40%以上,NT-proBNP水平升高,存在结构性心脏病并伴有生活质量下降,患者随机接受沙库巴曲缬沙坦钠(n=1286)或其他肾素-血管紧张素系统药物(单独使用沙库巴曲、单独使用缬沙坦或安慰剂,n=1286)。研究的主要终点为第12周血浆NT-proBNP水平和第24周6分钟步行距离变化,次要终点是24周时生活质量和纽约心脏协会(NYHA)分级变化。
患者平均年龄72.6岁,1301名女性(50.7%),2240人(87.1%)完成了试验。基线检查时,沙库巴曲缬沙坦钠组的NT-proBNP平均水平为786 pg/mL,对照组为760 pg/mL。12周后,沙库巴曲缬沙坦钠组NT-proBNP下降更为显著(调整后几何平均值与基线值差异为0.82 vs 0.98 pg/mL)。在第24周,沙库巴曲缬沙坦钠组和对照组6分钟步行距离分别增加了9.7米和12.2米(调整后的平均差异,-2.5m),差异不显著。组间堪萨斯城心肌病问卷临床总结得分变化(12.3 vs 11.8;平均差异为0.52)或NYHA改善患者比例(23.6% vs24.0%;调整后的优势比为0.98)无显著差异。与对照组相比,沙库巴曲缬沙坦钠组最常见的不良事件为低血压(14.1%vs5.5%)、蛋白尿(12.3%vs7.6%)和高钾血症(11.6%vs10.9%)。
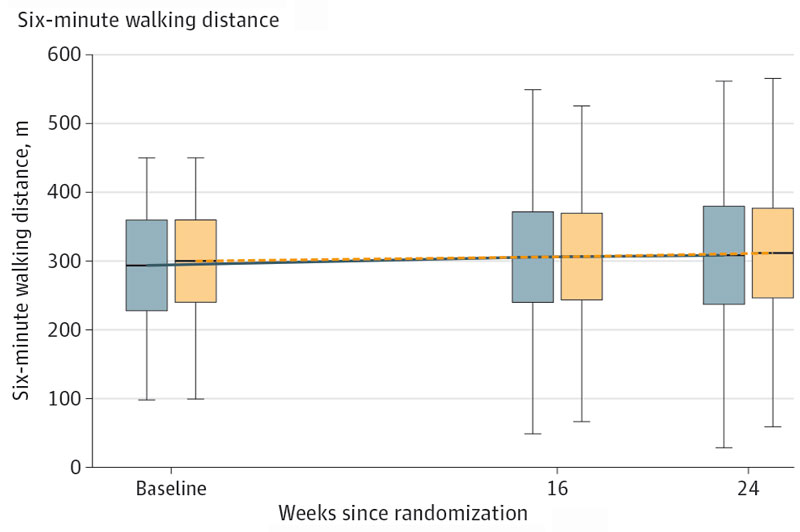
组间6分钟步行距离变化
研究认为,对于左室射血分数40%以上的心力衰竭患者,与标准的肾素-血管紧张素系统抑制剂治疗或安慰剂相比,沙库巴曲缬沙坦钠治疗可降低血浆N-末端脑钠肽前体水平,但对6分钟步行距离无显著改善作用。
原始出处:
Burkert Pieske et al. Effect of Sacubitril/Valsartan vs Standard Medical Therapies on Plasma NT-proBNP Concentration and Submaximal Exercise Capacity in Patients With Heart Failure and Preserved Ejection Fraction The PARALLAX Randomized Clinical Trial. JAMA. November 16,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
51
学习了
63
#缬沙坦#
46
#运动能力#
43
#沙库巴曲缬沙坦#
46
学习了!
50