NEJM:HLA不相容移植后免疫排斥的治疗
2017-08-03 zhangfan MedSci原创
研究认为酿脓链球菌内切酶可以减弱供体特异性抗体的作用,用于HLA不相容移植后免疫排斥的治疗
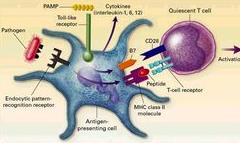
供体特异性抗体是导致排异反应的主要原因,对于HLA高度不相容移植者,现有的排异反应治疗效果效果不佳。肽链内切酶--源于酿脓链球菌(IdeS),可将人类IgG分解为F(ab')2和Fc片段,抑制补体和抗体依赖的细胞毒作用,具有潜在的缓解排异反应作用。近日研究人员开展了一项I-II期临床研究考察IdeS 用于HLA不相容供体肾移植后的脱敏治疗。研究招募了25名HLA敏感患者,在接受HLA不相容肾移植前进行了IdeS 治疗,对患者的不良事件、结果、供体特异性抗体和肾功能进行严密监控。移植后使用的免疫抑制剂包括他克莫司、霉酚酸酯、糖皮质激素。部分患者静脉注射免疫球蛋白和利妥昔单抗防止移植后排异反应。研究发现静脉注射免疫球蛋白和利妥昔单抗的患者,其冷缺血期显著延长、移植肾功能延迟恢复率较高以及I型供体特异性抗体水平较高。15名患者发生了38起严重不良事件,其中5起可能与IdeS相关。接受IdeS治疗后,IgG以及HLA抗体完全消除,24名患者进行了灌注移植,在移植后的2周至5个月内,10名患者进行了抗体介导排斥反应治疗,IdeS治疗的反应率为100%。研究认为酿脓链球菌内切酶可以减弱供体特异性抗
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#排斥#
33
#HLA#
31
#免疫排斥#
41
学习了,涨知识
67
好好文章学习了
62
学了。。。。。。。。。。。。
43
谢谢分享,学习了
72