PLoS Genet:三阴性乳腺癌与同源重组缺陷有关!
2017-06-27 Emma MedSci原创
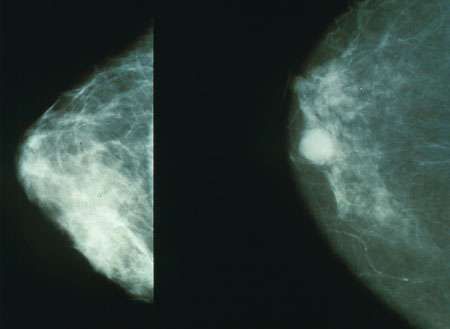
三阴性乳腺癌(TNBC)是指癌组织免疫组织化学检查结果为雌激素受体(ER)、孕激素受体(PR)和原癌基因Her-2均为阴性的乳腺癌。临床表现为一种侵袭性病程,其远处转移风险较高,内脏转移机会较骨转移高,脑转移几率也较高,预后较其他类型差。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#阴性乳腺癌#
36
#NET#
45
#Genet#
40
#同源重组#
43
#Gene#
31
#三阴性#
47