Hypertension:Resolvin E1通过抑制Wnt7a/β-Catenin信号减弱肺动脉高压
2021-11-02 刘少飞 MedSci原创
Resolvin E1通过抑制Wnt7a/β-Catenin信号减弱肺动脉高压。

肺动脉高压(PAH)是一种破坏性疾病,其特征是严重的肺血管壁重塑和血管周围炎症。
Resolvin E1 (RvE1) 是一种有效的促炎症反应介质,衍生自 omega-3 脂肪酸二十碳五烯酸 (EPA)。Resolvin E1 是在急性炎症的自发消退阶段 (存在特定的细胞间相互作用) 中,在阿司匹林存在下从 EPA 内源性生物合成的。Resolvin E1 具有独特的反调节作用,可以抑制多形核白细胞 (PMN) 跨内皮迁移。Resolvin E1 还可作为白细胞浸润,树突状细胞迁移和 IL-12 产生的有效抑制剂。然而,RvE1 对 PAH 发展的影响仍有待确定。该研究目的是检测RvE1 是否对 PAH 有治疗作用,如果有,则阐明其作用背后的分子机制。
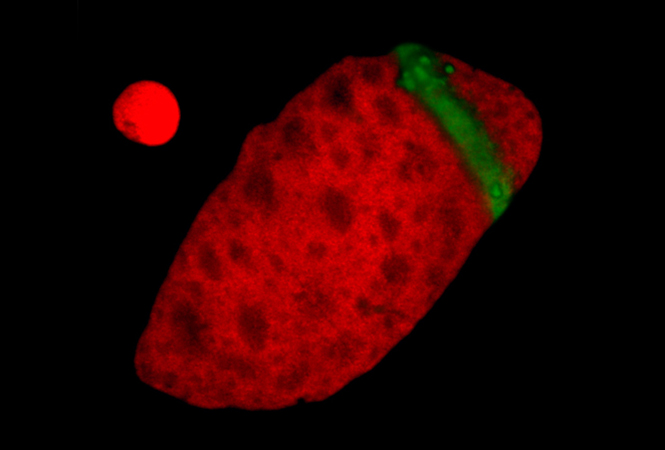
研究设计:首先,缺氧+SU5416诱导的肺动脉高压(PH)小鼠模型和野百合碱诱导的PH大鼠模型用于测试RvE1的治疗效果。其次,从患有 PAH 的患者和啮齿动物模型中收集肺组织和血浆样本,以检查 RvE1 的产生及其受体趋化因子趋化因子样受体 1 (ChemR23) 的表达。
研究结果:
该研究发现在特发性 PAH 患者的血浆和 PH 实验啮齿动物模型的肺中 RvE1 的生成减少。 ChemR23 表达在缺氧暴露的小鼠肺动脉平滑肌细胞 (PASMC) 和来自 PH 啮齿动物和特发性 PAH 患者的肺动脉中显着下调。 RvE1 可以通过抑制 PASMC 增殖减轻了雄性和雌性啮齿动物的实验性 PH。血管 SMC 中 ChemR23 的缺失消除了 RvE1 对小鼠缺氧+SU5416 诱导的 PAH 的保护作用。从机制上讲,RvE1/ChemR23 轴通过抑制增殖性无翼型 MMTV 整合位点家族成员 7a/β-catenin 信号传导来抑制缺氧诱导的 PASMC 增殖。 RvE1 对 ChemR23 的激活通过抑制蛋白激酶 A 介导的 Egr2(早期生长反应 2)在 Ser349 的磷酸化,减少了 PASMC 中无翼型 MMTV 整合位点家族成员 7a 的表达。

研究结论:
RvE1/ChemR23 轴通过调节 PASMC 中无翼型 MMTV 整合位点家族成员 7a/β-catenin 信号传导来抑制实验性 PAH,并可作为 PAH 管理的治疗靶点。
文章出处:
Liu G, Wan N, Liu Q, Chen Y, Cui H, Wang Y, Ren J, Shen X, Lu W, Yu Y, Shen Y, Wang J. Resolvin E1 Attenuates Pulmonary Hypertension by Suppressing Wnt7a/β-Catenin Signaling. Hypertension. 2021 Oct 25:HYPERTENSIONAHA12117809. doi: 10.1161/HYPERTENSIONAHA.121.17809. Epub ahead of print. PMID: 34689593.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#TENS#
27
#PE#
25
#动脉高压#
34
#ESO#
43
#Hypertension#
46
#WNT#
35