Sci Rep:静脉冲击注射甲基强的松龙联合小剂量强的松治疗高危IgA肾病
2022-01-19 从医路漫漫 MedSci原创
虽然IgAN的发病机制尚不完全清楚,但越来越多的证据表明,包括扁桃体感染和肠道感染在内的粘膜感染在IgAN的疾病进展中起着关键作用,遗传、环境和补体可能也参与了IgAN的发病机制。
虽然IgAN的发病机制尚不完全清楚,但越来越多的证据表明,包括扁桃体感染和肠道感染在内的粘膜感染在IgAN的疾病进展中起着关键作用,遗传、环境和补体可能也参与了IgAN的发病机制。半乳糖异常缺乏的IgA介导的免疫复合物沉积引起的肾小球炎症被认为在IgAN的发生发展中发挥了重要作用。
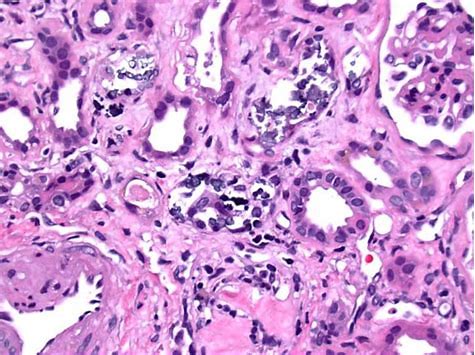
IgAN的临床表现和肾脏病理结果各不相同,这导致了不同的治疗选择和结果。大多数受影响的IgAN患者会发展为慢性和缓慢进展的肾损伤,其中大约30%的患者最终会发展到ESKD。持续性和大量蛋白尿,特别是蛋白尿> 1 g/d 和高血压被认为是预测肾功能下降的最广泛的两个危险因素。降低IgAN患者的蛋白尿水平通常被认为与较慢的肾功能下降和较低的ESKD风险相关。肾脏疾病:改善全球结局(KDIGO) 2021年肾小球疾病管理临床实践指南建议,当免疫抑制剂降蛋白尿治疗不能将尿蛋白水平降至1g/24小时以下时,高危IgA患者应考虑使用糖皮质激素,同时使用磺胺类药物预防糖皮质激素引起的潜在机会性感染。
大剂量强的松(FP)方案治疗高危免疫球蛋白A肾病(IgAN)患者仍存在争议。静脉冲击注射甲基泼尼松龙联合小剂量泼尼松(MCALP)可能具有更有利的安全性,这一点尚未得到充分研究。
方法:87例经活检证实的IgAN成人患者,在ACEI/ARB治疗至少90天后,蛋白尿在1 - 3.5 g/24小时之间,随机分配。(1)治疗组:在疗程开始时和第3个月分别静脉注射甲基泼尼松龙0.5 g,连续3天,每隔一天口服泼尼松15mg,连续6个月。(2)FP组:泼尼松0.8 ~ 1.0 mg/kg/d(最多70 mg/d),连续2个月,然后每10天减少5 mg/d,持续4个月。随访12个月。主要转归为12个月时蛋白尿完全缓解(CR)。
结果:MCALP组和FP组在第12个月和第18个月的CR比例相似(第12个月51% vs 58%, P = 0.490;60% vs 56%,第18个月P = 0.714)。MCALP组糖皮质激素累积剂量低于FP组(4.31±0.26 g vs 7.34±1.21 g, P < 0.001)。肾活检经牛津MEST - C评分与临床结果之间的相关性分析表明,有或没有M1、E1、S1、T1/T2和C1/C2的两组患者的总缓解率相似。更多的FP组患者出现感染(MCALP为8%,FP为21%)、体重增加(MCALP为4%,FP为19%)和库欣综合征(MCALP为3%,FP为18%)。
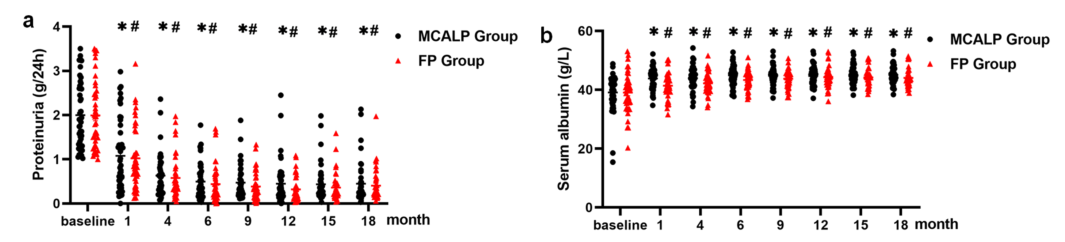
图1 随访时蛋白尿和血清白蛋白的变化。(A)蛋白尿比较。(B)血清白蛋白比较。数据显示在基线、1、4、6、9、12、15和18个月的随访中。*或#分别与基线比较,每一次随访均P<0.05。
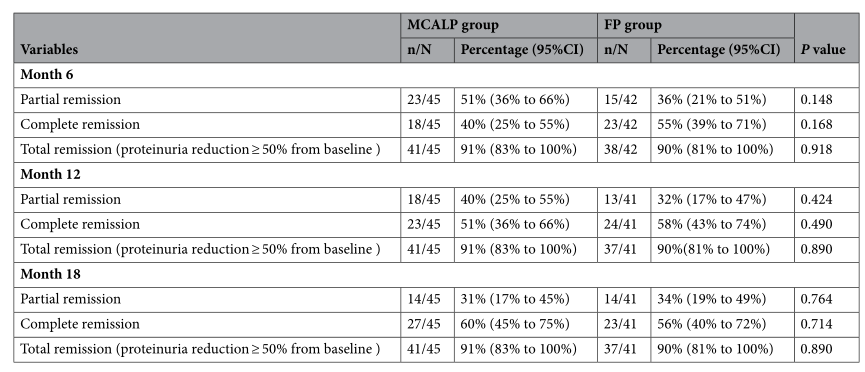
表1 观察两组治疗后第6、12、18个月的部分缓解、完全缓解和总缓解率。CI,置信区间。N/N表示事件数量/总数。
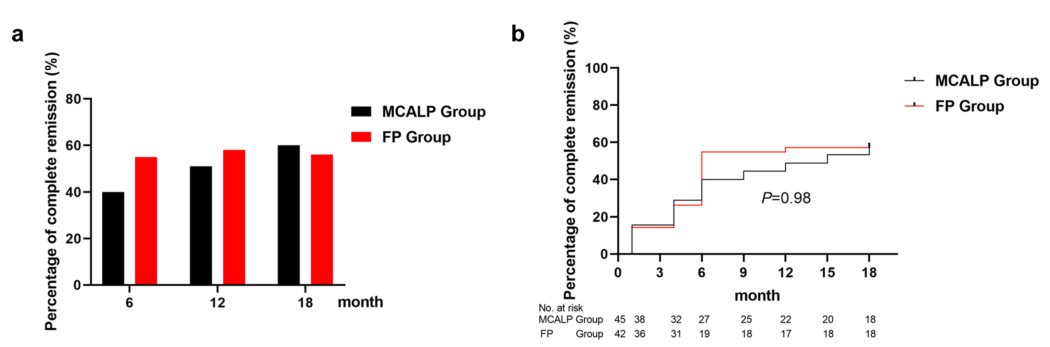
图2 随访中临床缓解期的变化。(A)治疗后6、12、18个月的完全缓解率。(B)完全缓解的Kaplan-Meier分析。
结论:这些数据表明,MCALP可能是进展为ESKD高风险的IgAN患者的可选择治疗方案之一。
原文出处: Li Y, Fu R, Gao J,et al.Effect of pulsed intravenous methylprednisolone with alternative low-dose prednisone on high-risk IgA nephropathy: a 18-month prospective clinical trial.Sci Rep 2022 Jan 07;12(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#静脉#
54
#强的松#
46
#小剂量#
40
#IgA肾病#
42
#IgA#
37
#甲基强的松龙#
56