JAHA:心力衰竭患者的电解剖比率与死亡率
2021-03-14 MedSci原创 MedSci原创
根据体形或左心室大小标准化的QRSd电解剖比与射血分数降低的心力衰竭患者的死亡率有关。特别是,QRS/身高比值升高可能是射血分数降低的心力衰竭患者的高危标志,QRS/左心室舒张末期容量可能进一步将识。
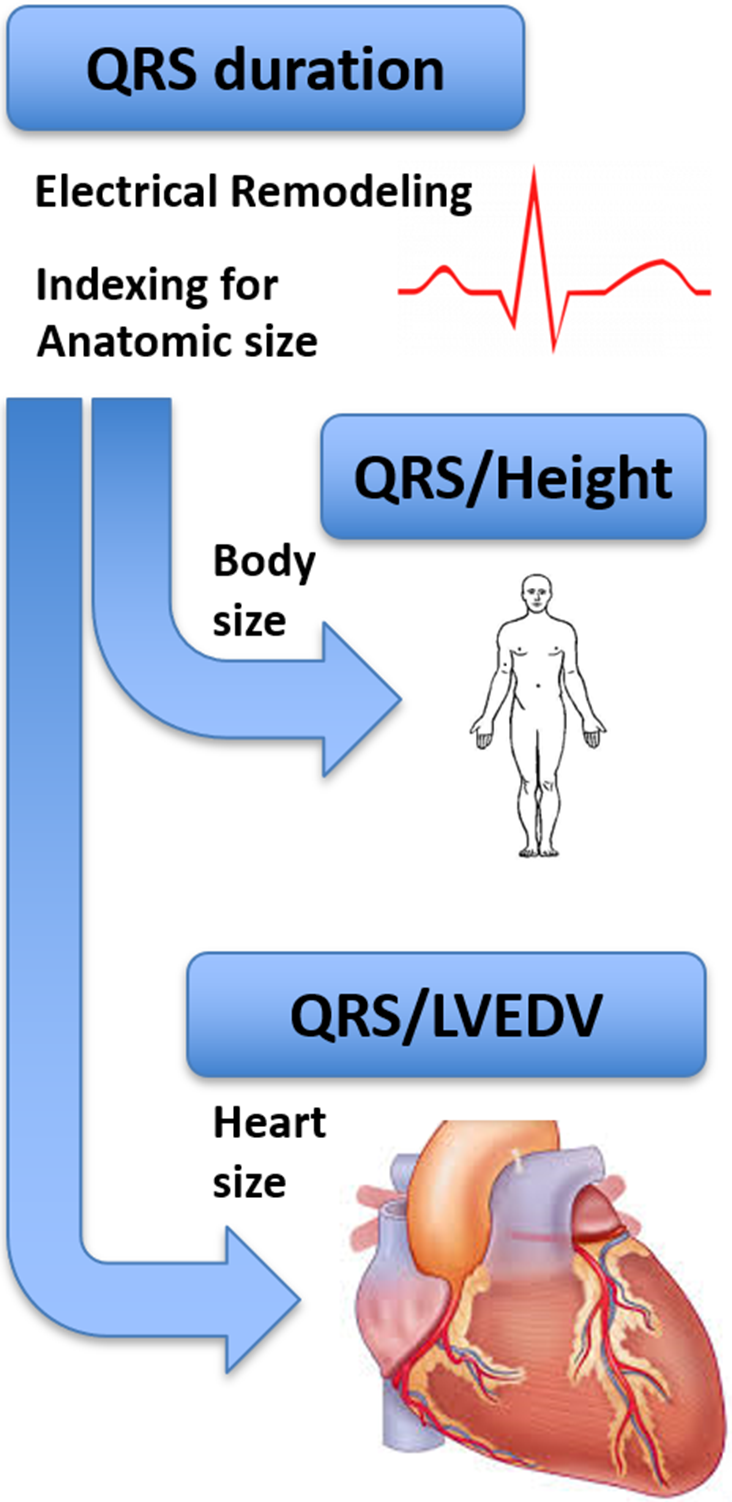
QRS持续时间(QRSd)是心力衰竭患者电重构的标志。人体测量学指标和左心室大小可能会影响QRSd,进而可能影响QRSd与心力衰竭结局之间的关联。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员通过前瞻性、多中心、跨国的ASIAN-HF(亚洲心衰猝死)登记中心,评估了心脏射血分数降低的心力衰竭患者的电解剖比率(以身高或左心室舒张末期容积标准化后的QRSd)是否与患者1年死亡率相关。

该研究纳入了4899名受试者(年龄60±19岁,男性78%,平均左心室射血分数:27.3±7.1%)。在整个队列中,QRSd与全因死亡率(风险比[HR]为1.003;95%CI为0.999-1.006,P=0.142)或心源性猝死(HR为1.006;95%CI为1.000-1.013,P=0.059)无关。QRS/身高与全因死亡率(HR为1.165;95%CI为1.046-1.296,P=0.005)和心源性猝死(HR为1.270; 95%CI为1.021-1.580,P=0.032)相关。
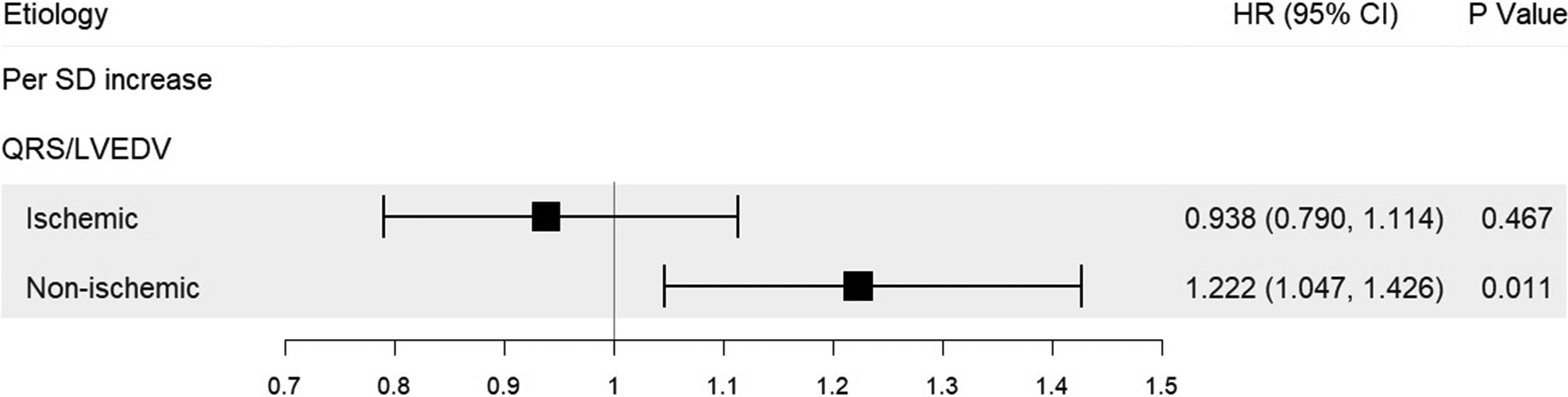
在非缺血性心肌病患者中,QRS/左心室舒张末期容积与全因死亡率(HR为1.22; 95%CI为1.05-1.43,P=0.011)和心源性猝死(HR为1.461; 95%CI为1.090-1.957,P=0.011),而在缺血性心肌病患者中则不然(全因死亡率:HR为0.94; 95%CI为0.79-1.11,P=0.467;心源性猝死:HR为0.734; 95%CI为0.477-1.132,P=0.162)。
由此可见,根据体形或左心室大小标准化的QRSd电解剖比与射血分数降低的心力衰竭患者的死亡率有关。特别是,QRS/身高比值升高可能是射血分数降低的心力衰竭患者的高危标志,QRS/左心室舒张末期容量可能进一步将识别出非缺血性射血分数降低的心力衰竭患者。
原始出处:
Janice Y. Chyou.et al.Electroanatomic Ratios and Mortality in Patients With Heart Failure: Insights from the ASIAN‐HF Registry.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.017932
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









把汉拿山
67
把v啊爸爸好
59
已读,真是受益匪浅呀。
91
#AHA#
39
保持关注
0