Oncotarget:强磁场科学中心在小细胞肺癌靶向治疗研究中取得进展
2017-07-20 李红 中国科学院强磁场科学中心
近日,强磁场科学中心林文楚研究员课题组在小细胞肺癌靶向治疗研究领域取得重要进展,相关研究成果以“Combination treatment of RAD001 and BEZ235 exhibits synergistic antitumor activity via down-regulation of p-4E-BP1/Mcl-1 in small cell lung cancer”为题,在线
近日,强磁场科学中心林文楚研究员课题组在小细胞肺癌靶向治疗研究领域取得重要进展,相关研究成果以“Combination treatment of RAD001 and BEZ235 exhibits synergistic antitumor activity via down-regulation of p-4E-BP1/Mcl-1 in small cell lung cancer”为题,在线发表在国际肿瘤学学术期刊《Oncotarget》上。
小细胞肺癌是肺癌中恶性程度最高的一种亚型,约占肺癌病人的15%-20%。小细胞肺癌分化程度低、倍增时间短、转移早且广泛、对化疗敏感但极易发生耐药。与非小细胞肺癌不同,目前没有有效的靶向治疗药物应用于小细胞肺癌的临床治疗。该研究发现两种小分子抑制剂(BEZ235和RAD001)的联合使用能显着地抑制小细胞肺癌的生长。

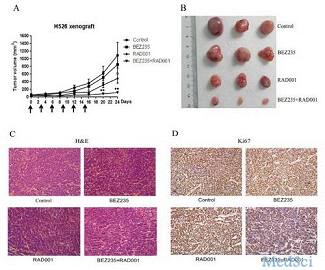
图:BEZ235和RAD001的联合使用显著地抑制H526小细胞肺癌小鼠移植瘤的生长
课题组通过挖掘癌症基因突变数据库,发现PI3K/AKT/mTOR信号通路在92%的小细胞肺癌细胞系中是不正常的。他们利用两药联用的方法,尝试了多种药物的组合,发现BEZ235(PI3K和mTOR双重抑制剂)和RAD001(mTOR抑制剂)的联合使用有效地抑制小细胞肺癌细胞和小鼠移植瘤的生长。在机制上,他们发现BEZ235和RAD001联合使用是通过抑制p-4E-BP1和Mcl-1蛋白进而抑制癌细胞的增殖。并且,课题组还发现4E-BP1的磷酸化的水平与BEZ235和RAD001对小细胞肺癌细胞的敏感性显着相关。这项研究工作不仅表明BEZ235和RAD001联合使用可能是一种有效地治疗小细胞肺癌的方法,并且发现磷酸化的4E-BP1可以作为BEZ235和RAD001治疗小细胞肺癌响应的生物标志物,具有潜在的临床应用价值。
原始出处:
Haiming Dai,Vivian Wai Yan Lui,Wenchu Lin.et al.Combination treatment of RAD001 and BEZ235 exhibits synergistic antitumor activity via down-regulation of p-4E-BP1/Mcl-1 in small cell lung cancer.Oncotarget.
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肺癌靶向治疗#
43
#target#
33
签到学习了很多人
81
学习了不错啊
79