Arthritis Rheumatol:系统性硬化症中尺动脉闭塞与血管病变严重程度标志物
2018-12-16 xiangting MedSci原创
UAO可作为SSc血管病变严重程度的相关标志物。
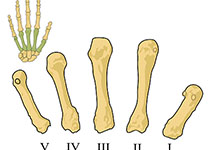
这项研究旨在评估通过多普勒超声(dUS)检测的尺动脉阻塞(UAO)与系统性硬化症(SSc)严重程度标志物的相关性。
这是一项横断面多中心研究,纳入符合SSc 2013 ACR/EULAR分类标准的204名未选择患者。根据现行指南,所有患者均可从评估是否存在UAO的双手dUS和临床/亚临床内脏评估中获益。建立单因素和多因素等级回归模型,将UAO的严重程度分级为"无UAO"、"仅1个UAO"和"双手UAO",并评估其与SSc临床特征的关联。
76名患者(37.3%)发现有UAO,49名为双侧(24.0%)。UAO作为等级事件与病程、指尖溃疡病史、毛细血管扩张、Rodnan皮肤评分较高、DLCO值较差、三尖瓣射流速度较高、晚期毛细血管镜类型和抗着丝粒抗体(ACA)阳性显著相关(单因素分析)。在调整后的多因素等级模型中,UAO在女性(OR=0.35 [0.15-0.83]; p=0.017)和使用类固醇的患者中较少发生(OR=0.24 [0.09-0.62]; p=0.0034)。在多因素分析中,指尖溃疡病史(OR=2.55 [1.24-5.21]; p=0.011)、Rodnan皮肤评分较高(OR=1.65 [1.06-2.56]; p=0.025)、DLCO较低(OR=0.85 [0.78-0.94]; p=0.0015)和ACA阳性(OR=2.89 [1.36-6.11]; p=0.0056)仍与UAO显著相关。
UAO可作为SSc血管病变严重程度的相关标志物。其对出现严重血管症状如肺动脉高压的预测价值,及其与死亡率的关联仍有待进一步纵向研究。
原始出处:
Alain Lescoat. Ulnar Artery Occlusion and severity markers of vasculopathy in Systemic sclerosis: a multicenter cross‐sectional study. Arthritis Rheumatol. 15 December 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#系统性#
28
#标志物#
25
#血管病#
25
#Arthritis#
33
#动脉闭塞#
27
#硬化症#
28
#ART#
27
#血管病变#
26
#系统性硬化#
29
感谢小编为我们准备了如此丰盛的精神大餐,同时也向作者致谢!认真学习了,点赞!
62