Gastric Cancer: 阿司匹林与胃腺癌术后长期生存的关系
2022-02-19 yd2015 MedSci原创
有研究表明,小剂量阿司匹林的使用可能降低癌症发病率和死亡率,但其对胃腺癌生存的影响尚不清楚。国外团队开展了相关研究,旨在评估在胃腺癌胃切除术后服用阿司匹林是否能改善长期生存。相关结果发表在Gastri
有研究表明,小剂量阿司匹林的使用可能降低癌症发病率和死亡率,但其对胃腺癌生存的影响尚不清楚。国外团队开展了相关研究,旨在评估在胃腺癌胃切除术后服用阿司匹林是否能改善长期生存。相关结果发表在Gastric Cancer杂志上。
这项以人群为基础的队列研究包括了2006年至2015年瑞典胃腺癌而行胃切除术的患者,并在整个2020年进行了随访。术前1年、2年、3年及胃切除术后1年暴露于每日低剂量(75-160 mg)阿司匹林与5年全因死亡率(主要结局)和疾病特异性死亡率相关。多变量Cox回归分析提供了95%可信区间(CI)的危险比(HR),调整了年龄、性别、教育程度、历年、共病、他汀类药物使用、肿瘤位置、肿瘤分期、新辅助化疗、胃切除手术的外科医生数量和手术根治性。
研究纳入2025例患者中,其中545例(26.9%)患者在手术时使用阿司匹林。在服用阿司匹林的患者中,178人(32.7%)术后没有再服用阿司匹林。约56例(2.8%)患者在胃切除术后一年内开始使用阿司匹林。52例(9.5%)阿司匹林服用者和91例(6.2%)非阿司匹林服用者在手术90天内死亡。
Kaplan–Meier曲线表明,服用和未服用阿司匹林患者的生存没有统计学差异。
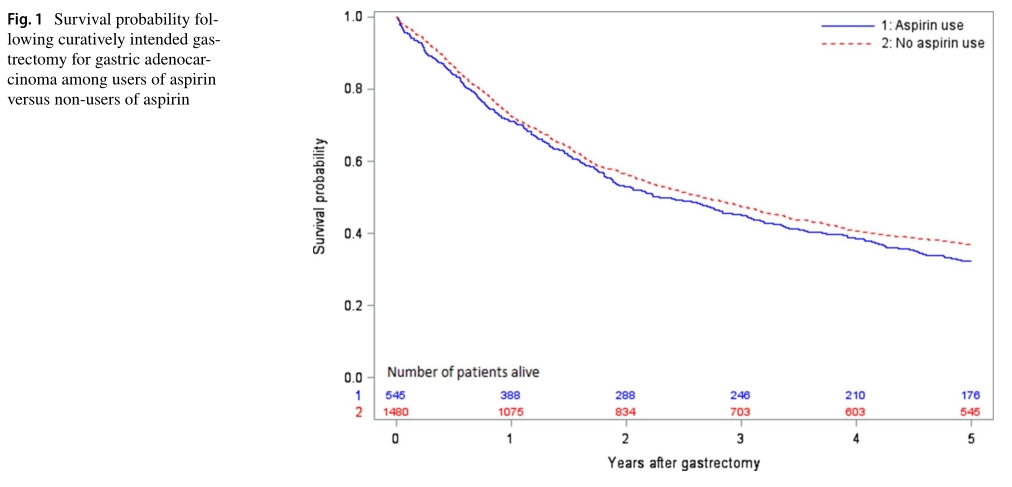
术前1年内使用阿司匹林并没有降低调整后的5年全因死亡率(HR = 0.98, 95% CI 0.85-1.13)或疾病特异性死亡率(HR = 1.00, 95% CI 0.86-1.17)风险。

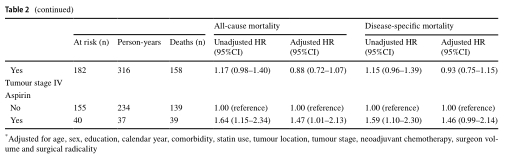
术前2年内(HR = 0.98, 95% CI 0.84-1.15)或3年内(HR = 0.94, 95% CI 0.79-1.12)服用阿司匹林并没有降低5年全因死亡率的风险。同样,术前和术后1年使用阿司匹林的患者,5年全因死亡风险均未出现任何降低(校正后HR=1.01, 95% CI 0.82-1.25)。
在敏感性分析中,我们排除了291例(14.3%)没有明确治疗目的的胃切除术患者。在对1734名患者的分析中,90天的死亡率为4.0%。与未服用阿司匹林者相比,服用阿司匹林与5年全因死亡率(调整后的HR=0.92, 95% CI 0.78-1.09)或5年疾病特异性死亡率(调整后的HR=0.94, 95% CI 0.79-1.13)均无相关性。
综上,研究表明,小剂量阿司匹林的使用可能不会提高胃腺癌术后的长期生存率。
原始出处:
Holmberg D, Kauppila JH, Mattsson F, Asplund J, Leijonmarck W, Xie SH, Lagergren J. Aspirin use in relation to long-term survival after gastrectomy for gastric adenocarcinoma. Gastric Cancer. 2022 Feb 15. doi: 10.1007/s10120-022-01282-0. Epub ahead of print. PMID: 35166957.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AST#
34
#GAS#
37
#gastric#
36
#胃腺癌#
42
#长期生存#
40