Ann Surg:切口iNPWT可降低术后伤口并发症的发病风险
2020-08-20 MedSci原创 MedSci原创
2016年WHO关于使用iNPWT预防SSI的建议是基于低水平的证据,此后许多试验相继发表。临床前证据表明,iNPWT还可以预防伤口开裂、皮肤坏死、血清肿和血肿。本研究旨在评估iNPWT预防术后伤口并
2016年WHO关于使用iNPWT预防SSI的建议是基于低水平的证据,此后许多试验相继发表。临床前证据表明,iNPWT还可以预防伤口开裂、皮肤坏死、血清肿和血肿。本研究旨在评估iNPWT预防术后伤口并发症(如SSI)的疗效。

在PubMed、EMBASE、CINAHL和CENTRAL中搜索比较iNPWT和对照敷料的随机和非随机研究。使用Cochrane偏倚风险工具、Newcastle-Ottawa量表和GRADE评估证据。使用随机效应模型进行了荟萃分析。
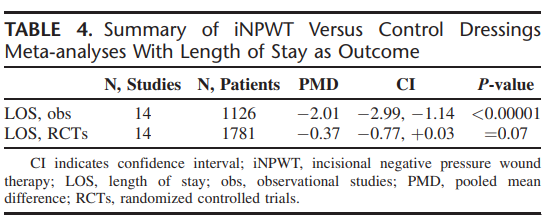
结果,高水平证据表明,iNPWT减少了SSI[28项RCTs,n = 4398,相对风险(RR)0.61,95%置信区间[CI]:0.49-0.76,P <0.0001,I = 27%],需要治疗的数量为19次。低水平证据表明,iNPWT可减少伤口开裂(16项RCTs,n = 3058,RR 0.78,95% CI:0.64-0.94)。很低水平的证据表明,iNPWT还减少了皮肤坏死(RR 0.49,95% CI:0.33-0.74)、血清瘤(RR 0.43,95% CI:0.32-0.59)和住院时间(汇总平均差异-2.01,95% CI:-2.99至1.14)。
总之,高水平的证据表明,切口iNPWT可降低SSI风险,且异质性有限。低至极低水平的证据表明,iNPWT还能降低伤口开裂、皮肤坏死和血清瘤的风险。
原始出处:
Pieter R Zwanenburg, Berend T Tol, et al., Meta-analysis, Meta-regression, and GRADE Assessment of Randomized and Nonrandomized Studies of Incisional Negative Pressure Wound Therapy Versus Control Dressings for the Prevention of Postoperative Wound Complications. Ann Surg. 2020 Jul;272(1):81-91. doi: 10.1097/SLA.0000000000003644.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NPWT#
39
👍
0
#并发#
37
值得学习及推荐
79
日常签到,赚点积分#学习#
94