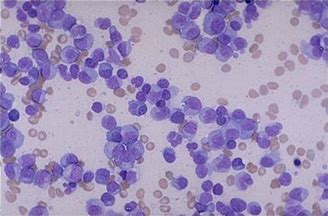
Leukemia:DNMT3A突变的转录水平并不能预测急性髓系白血病患者的结局
2018-01-23 MedSci MedSci原创
达到完全缓解是患者治愈或长期生存的不可或缺的先决条件。形态学上的完全缓解,即骨髓原始细胞<5%,对临床医生来说仍是有效的评估诱导治疗效果的必需信息。
达到完全缓解是患者治愈或长期生存的不可或缺的先决条件。形态学上的完全缓解,即骨髓原始细胞<5%,对临床医生来说仍是有效的评估诱导治疗效果的必需信息。
科学家们为了寻找DNMT3Amut是否能够作为微小残留病灶(minimal residual disease,MRD)监测,以及预测AML患者治疗结局的分子标志。通过实时定量聚合酶链式反应检测了1494个样本,而这些样本是从181例接受高强度治疗,并且存在DNMT3A在密码子R882(R882H;R882C)两个突变中的一个的病人中获得的。
在疾病诊断时,DNMT3A突变转录水平与目前的临床疾病特征,同时发生的基因突变,以及生存终点没有明显的相关性。在Cox回归分析汇总显示骨髓DNMT3Amut转录水平与复发或死亡率不相关。在诱导期Ⅰ,诱导期Ⅱ和巩固期Ⅰ,巩固期Ⅱ的DNMT3Amut转录水平在骨髓中显着高于血液。关于临床相关MRD时间点,在诱导两个循环之后,以及治疗后期,DNMT3Amut转录水平对终点缓和持续期以及整体生存没有明显的影响。值得注意的是,仅有一小部分的病人达到了PQ-PCR检测阴性,并且大部分病人都存在持续的高水平DNMT3Amut转录,而这个研究结果表明在血液缓解期,克隆性造血持续存在。
本文出处:Gaidzik V I, Weber D, Paschka P, et al. DNMT3A mutant transcript levels persist in remission and do not predict outcome in patients with acute myeloid leukemia[J]. Leukemia, 2017.doi:10.1038/leu.2017.200
本文由梅斯医学(MedSci)原创编译整理,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#髓系白血病#
37
#转录#
37
#DNMT3A突变#
42
#DNMT3A#
36
henhao
76
henhao
69